Das geschulte Auge eines Beatmungsexperten ist in der Lage, Asynchronitäten zu erkennen, indem es die Formen der Flow- oder Druckkurven analysiert.
Der Zustand des Patienten kann sich jedoch von einem Atemzug auf den anderen verändern, und der Experte kann nicht ständig am Patientenbett sein.
An dieser Stelle kommt IntelliSync+ ins Spiel. Diese Technologie übernimmt die Funktion des Expertenauges und erkennt anhand der Kurven Anzeichen einer Atembemühung (Trigger) oder Entspannung (Einleiten der Exspiration) seitens des Patienten.
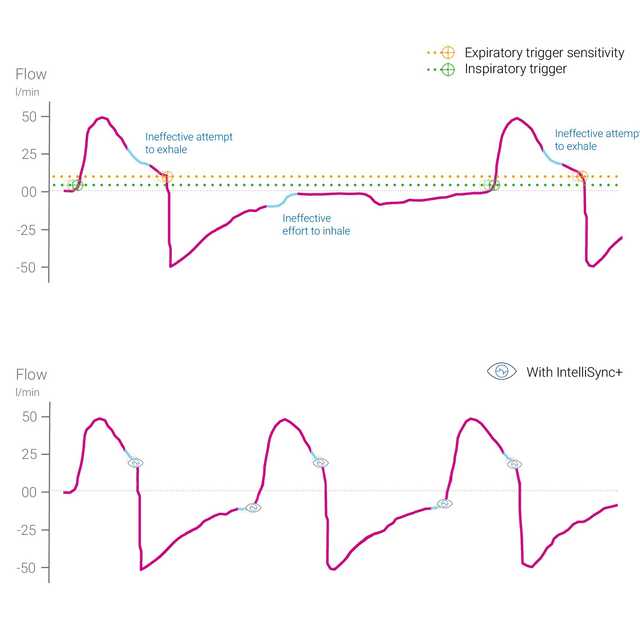
IntelliSync+ analysiert die Kurvensignale kontinuierlich, und zwar mindestens einhundert Mal pro Sekunde. Dadurch kann IntelliSync+ Patientenanstrengungen sofort erkennen und Inspiration und Exspiration in Echtzeit initiieren. Somit sind herkömmliche Triggereinstellungen für Inspiration und Exspiration überflüssig.
Für maximale Flexibilität können Sie IntelliSync+ entweder für den inspiratorischen Trigger oder den exspiratorischen Trigger oder für beide aktivieren.

Bei etwa 25 % aller maschinell beatmeter Patienten kommt es zu einer hohen Anzahl grösserer Asynchronien zwischen Patient und Beatmungsgerät (
Die Kurvenformanalyse ist eine zuverlässige, genaue und wiederholbare Methode zur Beurteilung der Interaktion zwischen Patient und Beatmungsgerät. Die Automatisierung dieser Methode kann eine kontinuierliche Überwachung von beatmeten Patienten und/oder eine Verbesserung der Atemtriggerung und Einleitung der Exspiration ermöglichen (
Mojoli F, Orlando A, Bianchi IM, et al.
Eine aktuelle Studie zeigte, dass die automatisierte Einleitung der Exspiration durch das Beatmungsgerät anhand der Echtzeitanalyse von Kurvenformen ein zuverlässiges Mittel ist, um die Synchronisation bei maschinell beatmeten Patienten zu verbessern.


IntelliSync+ ist eine durchwegs nichtinvasive Methode, für die keine zusätzliche Hardware oder Zubehör benötigt wird. Aktivieren Sie einfach die Option an Ihrem Beatmungsgerät, um sie in invasiven und nichtinvasiven Beatmungsmodi bei erwachsenen und pädiatrischen Patienten einzusetzen.
Da IntelliSync+ auch mit herkömmlichen Triggern kombiniert werden kann, haben Sie die Wahl, IntelliSync+ entweder während der Inspiration, der Exspiration oder bei beiden zu verwenden.

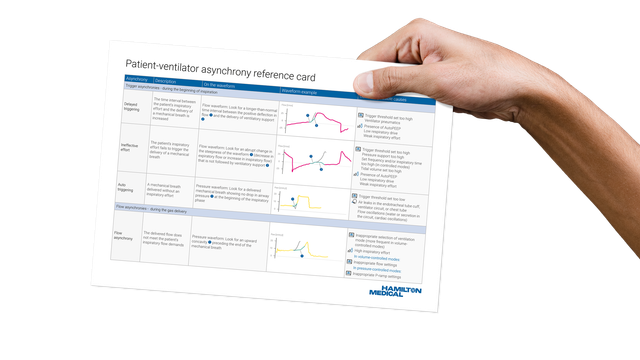
Unsere Übersichtskarte zu Asynchronien gibt Ihnen einen Überblick über die gängigsten Asynchronietypen, ihre Ursachen und wie Sie sie erkennen.
IntelliSync+ ist auf den Beatmungsgeräten HAMILTON-C6 und HAMILTON-G5 als Option verfügbar und gehört auf dem HAMILTON-S1 zu den Standardfunktionen.