El ojo entrenado de un experto en ventilación es capaz de detectar asincronías analizando las formas de onda de presión o de flujo.
Sin embargo, el estado del paciente puede cambiar entre una respiración y otra y el experto no siempre se encuentra en junto al paciente.
Aquí es donde toma el control el IntelliSync+. Esta tecnología imita el ojo experto para identificar los signos de esfuerzo (disparo) o de relajación (ciclado) del paciente en la forma de onda.
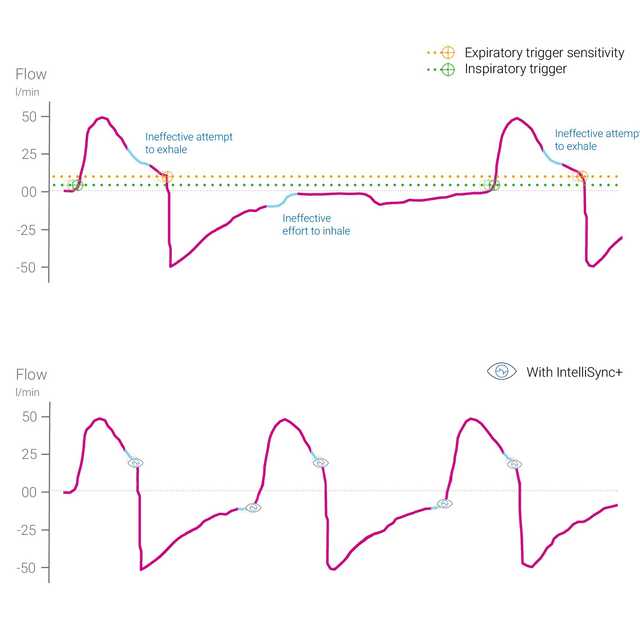
IntelliSync+ analiza de manera continua las señales de las formas de onda al menos cien veces por segundo. Esto permite a IntelliSync+ detectar el esfuerzo del paciente de manera inmediata e iniciar la inspiración y la espiración en tiempo real, lo que sustituye los ajustes de disparo de inspiración y espiración convencionales.
Para ofrecer la máxima flexibilidad, puede optar por activar IntelliSync+ para automatizar el disparo inspiratorio o el disparo espiratorio, o ambos.

Se observó un elevado número de asincronías importantes entre el paciente y el respirador en el 25 % de todos los pacientes con ventilación mecánica (
El análisis de formas de onda es un método fiable, preciso y reproducible para evaluar la interacción entre el paciente y el respirador. La automatización de este método permite una monitorización continua de los pacientes ventilados o una mejor activación de la respiración y del ciclado (
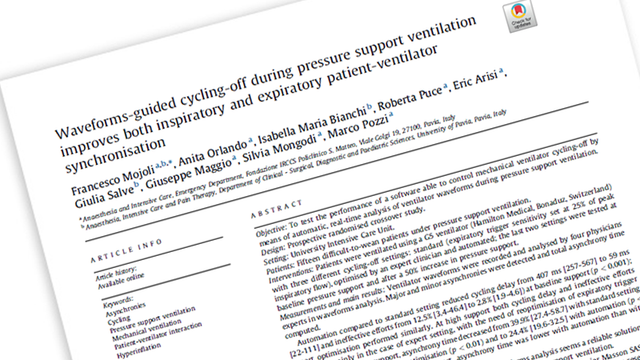
Mojoli F, Orlando A, Bianchi IM, et al.
Un estudio reciente mostró que el control automatizado de los ciclos de apagado inspiratorio del respirador basado en el análisis en tiempo real de las formas de onda proporcionó un medio fiable para mejorar la sincronización en pacientes con ventilación mecánica.


IntelliSync+ es un método completamente no invasivo que no requiere ningún accesorio ni hardware adicionales. Basta con activar la opción en el respirador para utilizarlo con los modos de ventilación invasiva o no invasiva en pacientes adultos y pediátricos.
Dado que IntelliSync+ también puede utilizarse en combinación con los disparos convencionales, tiene la posibilidad de elegir cuándo utilizar IntelliSync+, es decir, durante la inspiración, la espiración o con ambas.

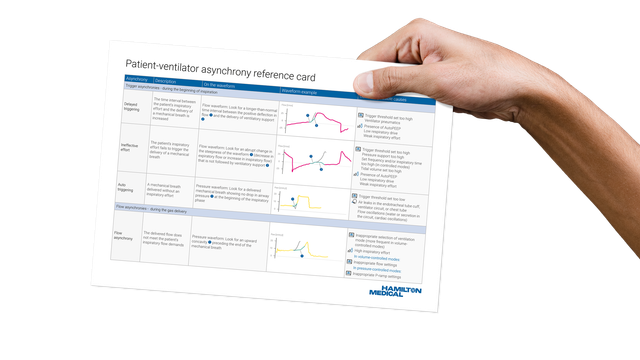
Nuestra hoja de referencia de asincronías incluye una descripción general de los tipos de asincronías más comunes, sus causas y cómo detectarlas.
IntelliSync+ está disponible de forma opcional para el HAMILTON-C6 y el HAMILTON-G5, y se incluye de serie en el HAMILTON-S1.