
Автор: Clinical Experts Group, Hamilton Medical
Дата: 05.11.2018
Last change: 05.11.2018
Psupport changed to Pinsp; addition of two screenshotsThe use of rapid sequence intubation (RSI) in the Emergency Department is often associated with complications, including serious oxygen desaturation.

The use of CPAP and/or NIV for preoxygenation may be particularly effective in reducing the risk of hypoxemia during intubation. A recent study from Australia now describes use of the HAMILTON-T1 to apply a combination of NIV and pressure-controlled ventilation in high-risk patients (
The authors' VAPOX technique (ventilator-assisted preoxygenation) is made possible by the HAMILTON-T1’s biphasic design and open valve system, which enable the application of NIV for preoxygenation followed by mechanical ventilation after intubation, all with the same breathing circuit.
After completing the preop tests and connecting the oxygen and power supplies, the HAMILTON-T1 is set up in NIV-ST mode with the following settings:
A nasal cannula is applied to the patient with an oxygen flow rate of 15 l/min and then a face mask is applied. The ventilator is started and preoxygenation applied for 3 minutes.
As soon as apnea ensues, the ventilator transitions to PCV+.
Intubation starts after at least 45 sec, with nasal oxygenation continuing until the ETT is in place.
With the tube successfully positioned, the ventilator can be switched to a conventional ventilation mode.


In this series of patients, there was no occurrence of hypoxia. The two patients with the lowest oxygen saturation at the outset (77% and 79%) increased to 100% and 94% post VAPOX, respectively, with values post intubation at 93% and 92%, respectively. These results showed VAPOX to be both safe and effective.
Using the HAMILTON-T1, this promising technique can successfully be applied to minimize hypoxemia during RSI.
Relevant devices: HAMILTON-T1
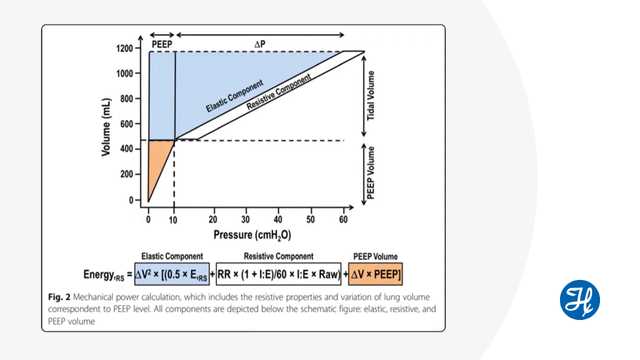
Mechanical power has become a hot topic in discussions about optimizing ventilator settings for critically ill patients.

In this article we outline the recommendations for the respiratory treatment of COVID-19 patients drawn from recent literature and guidelines issued by various organizations worldwide. They reflect the status as at the date of last change shown here.