Опытный специалист по ИВЛ способен определять асинхронности на глаз по формам кривых потока и давления.
Однако состояние пациента может меняться с каждым вдохом, а специалист не всегда находится рядом.
Именно в этом случае требуется функция IntelliSync+. Эта технология имитирует взгляд специалиста и обнаруживает признаки дыхательного усилия (триггер) и расслабления (циклирование) на кривой.
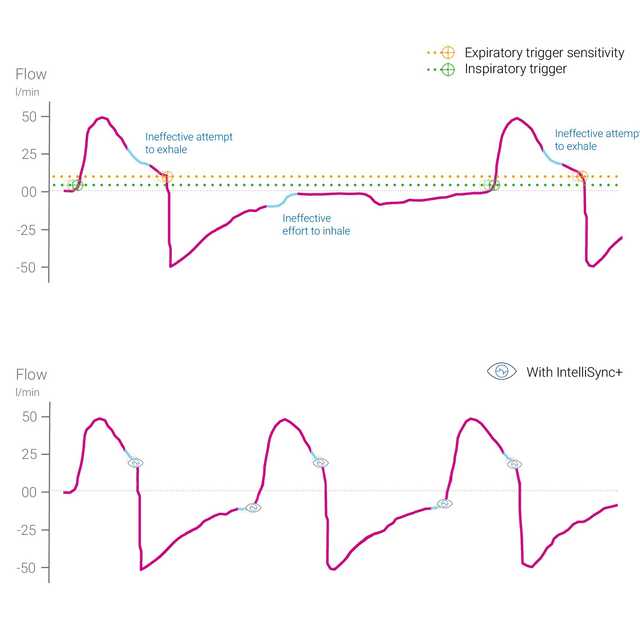
Функция IntelliSync+ непрерывно анализирует сигналы кривых не менее ста раз в секунду. Это позволяет функции IntelliSync+ немедленно обнаруживать дыхательные усилия пациента и инициировать вдох и выдох в реальном времени, тем самым заменяя обычные настройки триггера для вдоха и выдоха.
Чтобы обеспечить максимальную универсальность применения, функцию IntelliSync+ можно активировать для автоматического срабатывания триггера вдоха, триггера выдоха или их обоих.

Приблизительно у 25 % всех пациентов, находящихся на искусственной вентиляции легких, наблюдается большое количество серьезных асинхронностей с аппаратом ИВЛ (
Анализ кривых — это надежный, точный и простой способ оценки синхронизации аппарата ИВЛ с дыханием пациента. Автоматизация этого метода может обеспечить непрерывный мониторинг пациентов, находящихся на ИВЛ, и/или улучшить триггирование и циклирование дыхания (
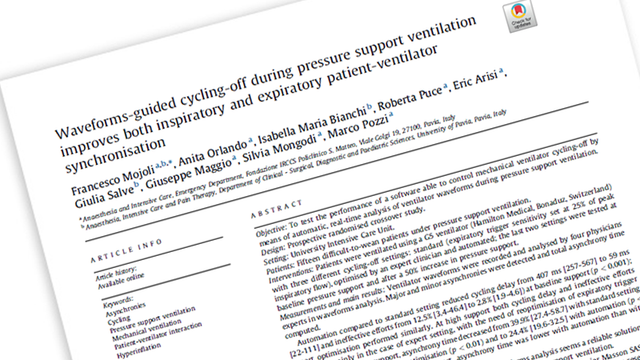
Mojoli F, Orlando A, Bianchi IM, et al.
Недавнее исследование показало, что автоматическое переключение аппарата ИВЛ со вдоха на выдох, выполняемое на основе анализа кривых в реальном времени, является надежным способом улучшения синхронизации дыхания пациентов при проведении искусственной вентиляции легких.


IntelliSync+ — это полностью неинвазивный метод, не требующий дополнительного оборудования или принадлежностей. Просто активируйте эту функцию на аппарате ИВЛ, чтобы использовать ее в режимах инвазивной и неинвазивной вентиляции у взрослых и педиатрических пациентов.
Поскольку функция IntelliSync+ также комбинируется с обычными триггерами, ее можно использовать для вдоха, выдоха или в обоих случаях.

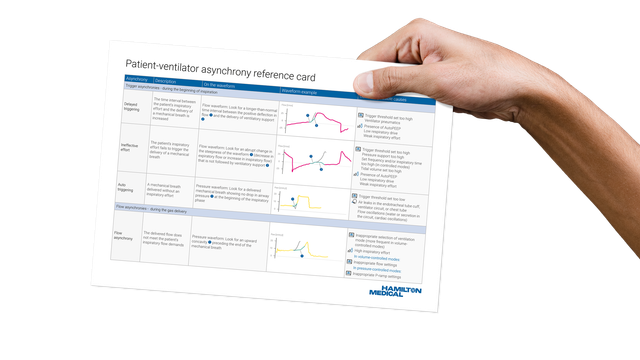
В справочной карте приведен обзор наиболее распространенных типов асинхронностей, а также описаны их причины и способы выявления.
Функция IntelliSync+ доступна как опция в аппаратах ИВЛ HAMILTON-C6 и HAMILTON-G5, а также является стандартной функцией в аппарате HAMILTON-S1.