作者: Clinical Experts Group, Hamilton Medical
日期: 30.08.2017
Driving pressure = Plateau pressure - Total PEEP
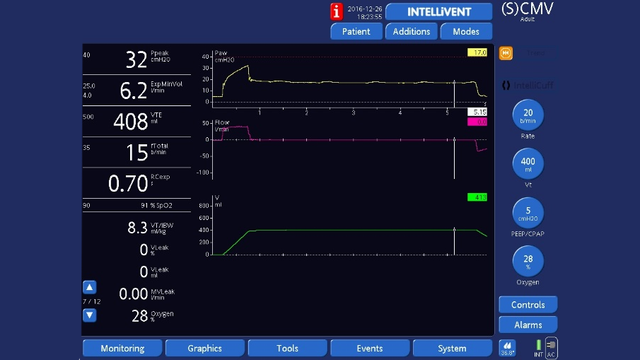
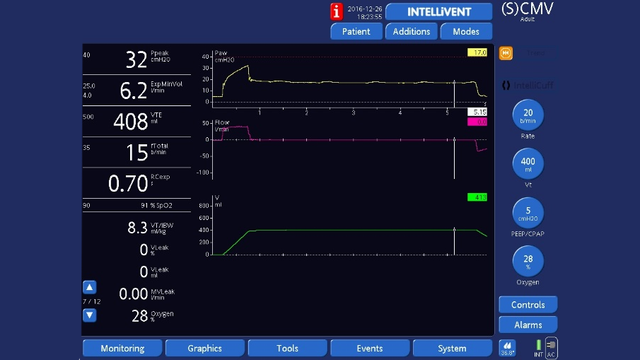
On a Hamilton Medical ventilator you can measure driving pressure in any ventilation mode, provided the patient is relaxed and making no inspiratory or expiratory effort, and there is no leakage from the ventilation circuit.
All you have to do is perform an end-inspiratory hold maneuver and then an end-expiratory hold for 3-5 seconds to measure the plateau pressure and total PEEP respectively.
So driving pressure = inspiratory hold pressure (plateau pressure) - expiratory hold pressure (total PEEP).
End-inspiratory hold: Press the Tools button to open the Tools -> Hold window and select Insp hold, wait for 3 to 5 seconds, then select Insp hold or press the P&T knob again to deactivate the hold maneuver and close the window. The waveforms will freeze so you can check that plateau pressure is stable, then measure pressure at the end of the plateau using the cursor.
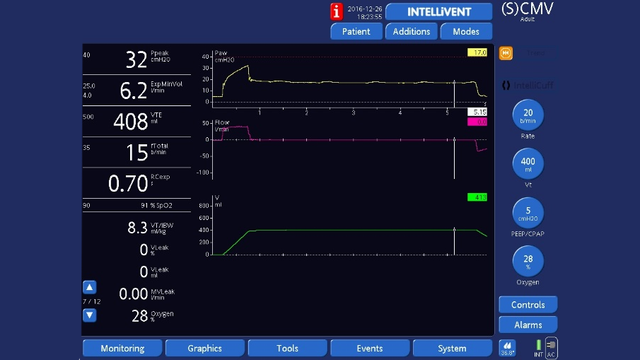
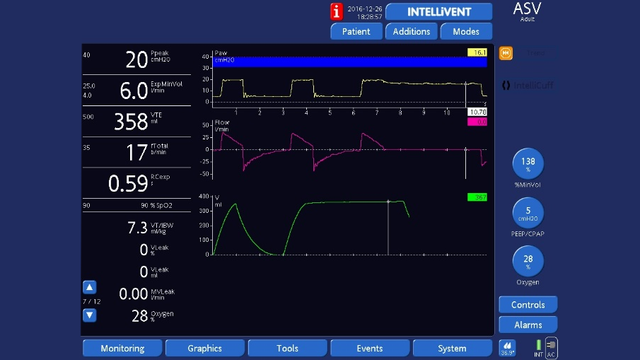
End-expiratory hold: As for end-inspiratory hold, but select Exp hold. Check that plateau pressure is stable, then measure pressure at the end of the plateau using the cursor.
Full citations below: (

