训练有素的通气专家眼睛可以通过分析流量或压力波形的形状来检测人机不同步。
但专家无法始终待在病人床旁,而且病人状况可能会随时改变。
这是 IntelliSync+ 的用途所在。此技术模拟专家的眼睛在波形上识别病人用力(触发)或放松(循环)的征象。
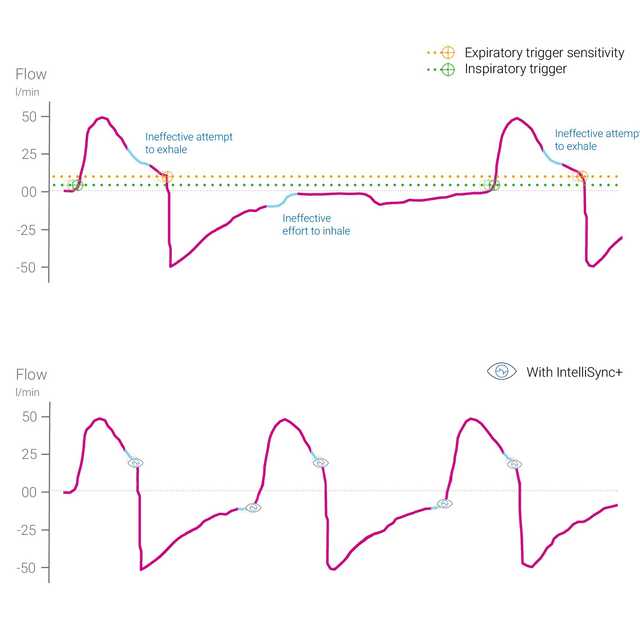
IntelliSync+ 至少每秒一百次连续分析波形信号。这使 IntelliSync+ 可以立即检测病人用力情况,并实时启动吸气和呼气,因此替代传统的吸气和呼气触发设置。
为了提供最大灵活性,您可以选择激活 IntelliSync+ 吸气触发或呼气触发或两者。

约 25% 的机械通气病人出现显著的人机异步性 (
波形分析是一种可靠、准确的可重复人机交互评估方法。此方法可以自动化运行,因此能够持续监测通气病人和/或改善的呼吸触发和循环 (
Mojoli F, Orlando A, Bianchi IM, et al.
最近的一项研究表明,基于波形实时分析的呼吸机循环自动控制提供了一种可靠的方法来改善机械通气病人的人机同步。


IntelliSync+ 是一种完全无创方法,它不需要任何额外的硬件或附件。您只需激活呼吸机上的选项,并在有创或无创通气模式下将其用于成人和儿童病人。
由于 IntelliSync+ 还可以与常规触发结合使用,您可以选择在吸气、呼气或两者期间使用 IntelliSync+。

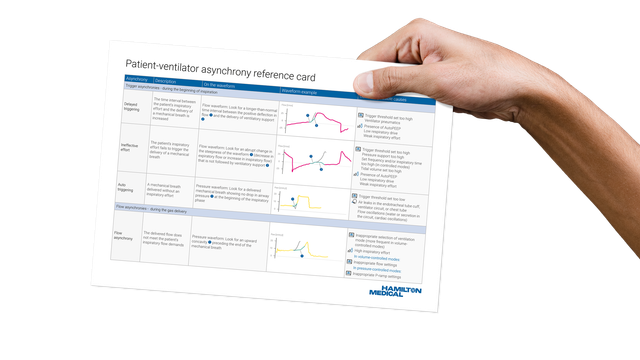
我们的异步参考卡向您概述了最常见的异步性类型、它们的原因以及如何检测它们。
IntelliSync+ 可作为 HAMILTON-C6 和 HAMILTON-G5 的选配功能及 HAMILTON-S1 的标准功能提供。