
无论设备用于 ICU、MRI 科室或病人转运,我们所有的呼吸机的用户界面操作方式均相同。
我们的通气酷屏将复杂的数据集成到直观的可视化图像。
一项研究发现单单数字和波形显示不足以为临床医生提供最佳支持 (
我们的通气酷屏受到飞机驾驶舱的启发,在飞机驾驶舱中,复杂数据被集成并以简化方式可视化。


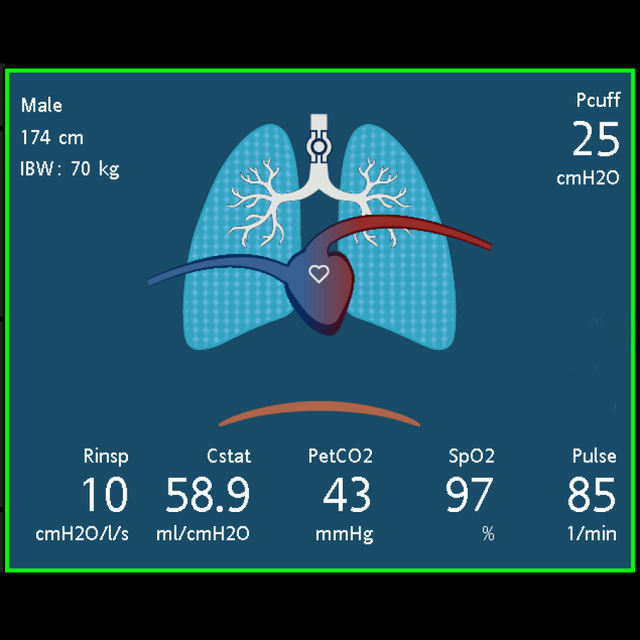

动态肺面板使以下监测数据实时可视化。如果所有值均在正常范围内,则该面板显示绿色边框。
基于近端流量传感器信号,肺与实际呼吸同步扩张和收缩。所显示的肺体积与基于病人身高的预期体积相关。
肺下方的动画膈膜显示病人自主活动。
如果集成气囊压力控制器 IntelliCuff 已连接并激活(
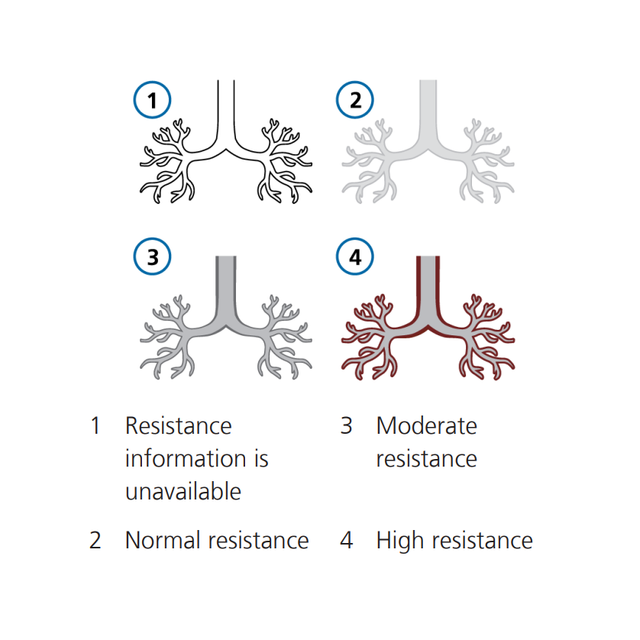
支气管树以逐次呼吸为基础显示与病人身高相关的阻力。支气管树的颜色显示阻力的相对程度。
同时显示数值。
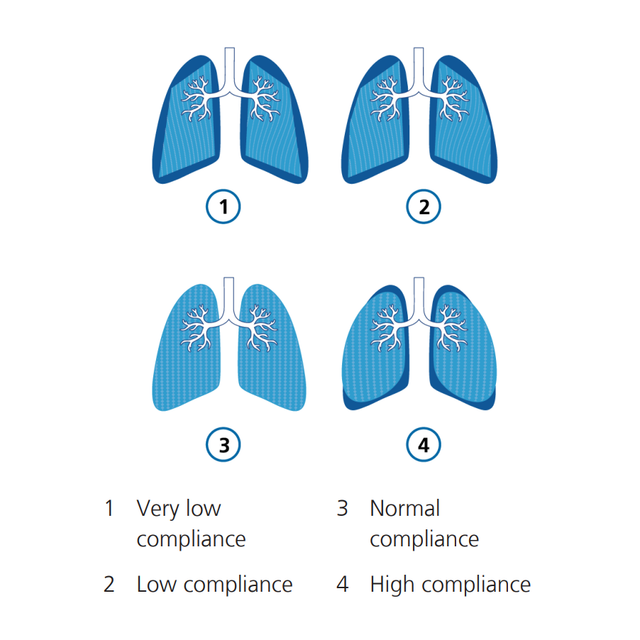
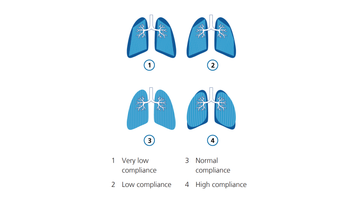
肺的形状每次呼吸随着与病人身高相关的顺应性 (Cstat) 变化。同时显示数值。
如果氧饱和度选项(
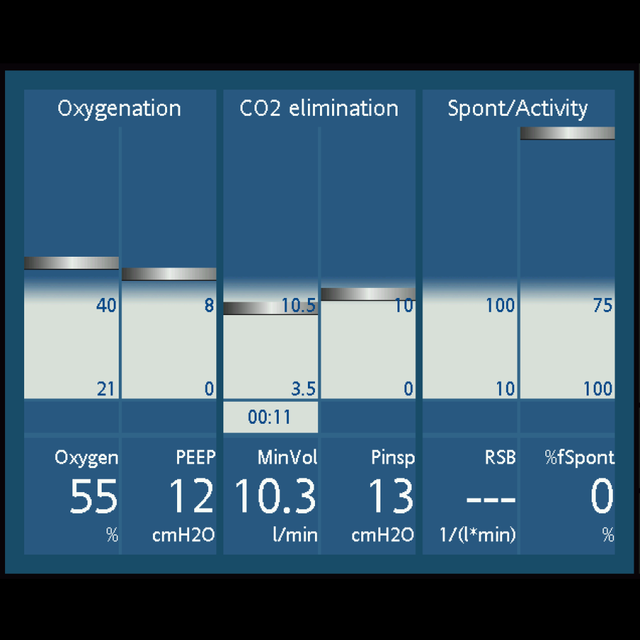
通气状态面板显示与病人的呼吸机依赖性相关的六个参数,包括氧合状态、CO2 清除状态和病人活动。
列中的浮动指示器按每次呼吸显示指定参数值。当指示器进入灰色撤机区域时,计时器开始显示该值位于撤机区域的时间。
当所有值都位于撤机区域内时,该面板显示绿色边框,表示可考虑尝试自主呼吸。

根据我的经验,动态肺十分有用,因为并不是每个人总能对数据有很好的解读,尤其是刚开始工作的治疗师。但他们能理解图片。
临床教育协调员
美国德克萨斯州拉伯克大学医疗中心
通气酷屏是我们所有重症监护呼吸机上的一项标准功能。