容积二氧化碳图的时相、形状和曲线形态和计算衍生的测量可以告诉您下列重要信息:
在我们的呼吸机上,使用病人气道近端的 CAPNOSTAT-5 主流式 CO2 传感器测量 CO2。
CAPNOSTAT-5 传感器针对呼气末二氧化碳分压 (PetCO2) 以及在 150 次/分钟下所有呼吸频率的清晰、准确的二氧化碳图提供准确的测量。
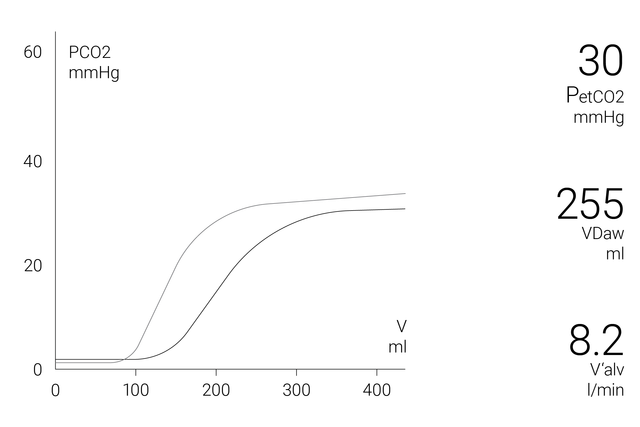
显示屏上的容积二氧化碳图窗口显示准确的定量信息作为近端流量和近端 CO2 数据的结合,例如:
为了解更多关于病人状况的综合分析,可获得以下参数的 72 小时趋势图(或 HAMILTON-S1/G5 呼吸机的 96 小时趋势图):
为了使您一目了然,Hamilton Medical 哈美顿医疗公司呼吸机在二氧化碳监测窗口提供了所有 CO2 相关性数据的概览。
学习如何解读容积二氧化碳图及了解容积二氧化碳图的优点和临床应用。包括自测内容!
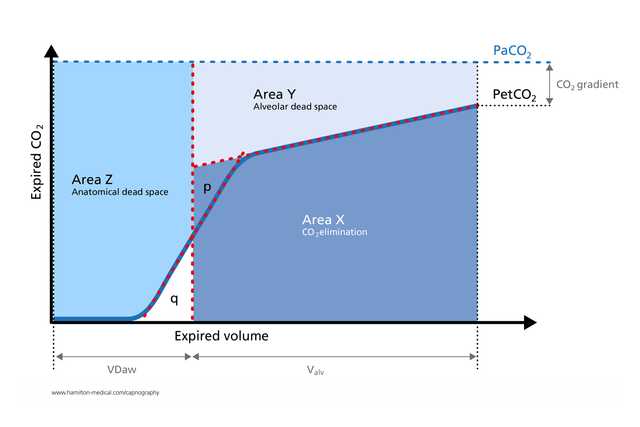
容积二氧化碳图已成功用于测量解剖死腔、肺毛细血管灌注和通气效率 (
容积二氧化碳图衍生计算有助于在床头识别肺动脉栓塞 (
接受机械通气的 ARDS 病人生理死腔-潮气量比的容积二氧化碳图测量与通过代谢监测技术获得的数据一样准确 (
呼气二氧化碳图是一种独立于呼吸努力、快速的无创测量,可帮助检测成人哮喘病人的显著支气管痉挛 (
容积二氧化碳图以无创、实时方式提供有关肺塌陷和肺复张生理学的宝贵见解,并有助于在床头监测周期性肺复张操作 (

我们提供成人、儿童和新生儿病人用原装耗材。您可根据您的机构政策选择可重复使用和一次性使用产品。
容积二氧化碳图可作为 HAMILTON-C6、HAMILTON-G5、HAMILTON-C3 和 HAMILTON-C1/T1 呼吸机的选配功能以及 HAMILTON-S1 呼吸机的标准功能提供。