Author: Jean-Michel Arnal, Senior Intensivist, Ste Musse Hospital, Toulon, France
Date of first publication: 23.04.2019
PEEP is used to keep the lung aerated and prevent lung collapse at the end of expiration. However, PEEP may over-distend the normally aerated lung and impair lung perfusion. Therefore, any change in PEEP may affect the overall ventilation/perfusion ratio in an unpredictable way.
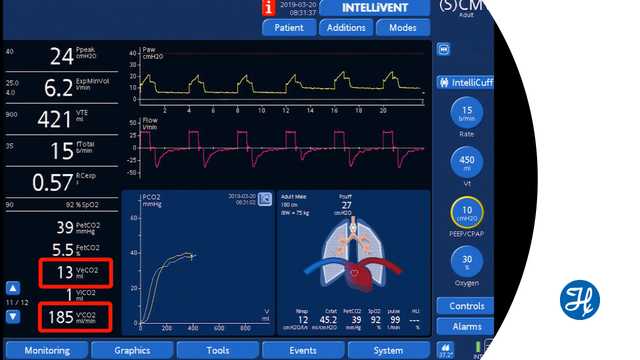
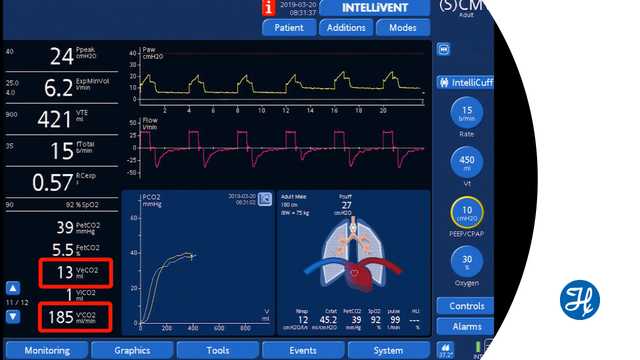
Volumetric capnography measures the volume of CO2 exhaled breath-by-breath (VeCO2). After a change in PEEP, assuming that the cardiovascular function and tidal volume are stable, an increase in VeCO2 means that the overall ventilation/perfusion ratio has improved. Conversely, a decrease in VeCO2 means that the ventilation/perfusion ratio is worsening. VeCO2 changes rapidly and returns to the baseline after a few minutes.
The limitation to this method is that the clinician monitors rapid changes to the ventilation/perfusion ratio, such as those due to lung over-distension and lung-perfusion impairment or improvement.
After a change in PEEP, recruitment or derecruitment may take a longer time to occur and cannot be assessed by this method.
Watch the video below to see a demonstration during ventilation with a Hamilton Medical ventilator.
Full citations below: (
Learn how to interpret a volumetric capnogram and get an overview of the benefits and clinical applications of volumetric capnography. Includes a self-test!