This article describes step-by-step how to set the ventilator when using the Adaptive Support Ventilation (ASV) mode on ARDS patients.
ASV targets the optimal respiratory rate for the low compliance of an ARDS patient and already targets low tidal volumes as recommended in the ARDS guidelines (
For any given minute volume, ASV determines the optimal respiratory rate and tidal volume associated with the minimal work of breathing and minimal driving pressure. It applies lung-protective ventilation with low tidal volumes (VT), and limited Pplateau and driving pressure in passive ICU patients with different lung conditions. In ARDS patients, ASV applies individualized lung-protective ventilation (
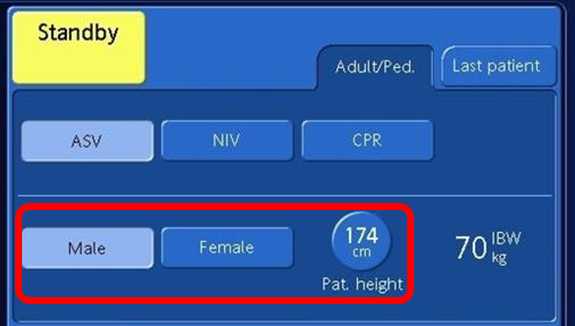
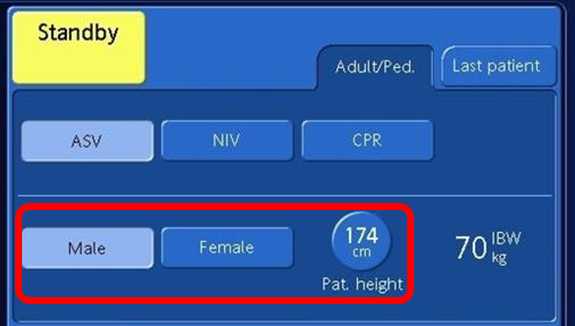
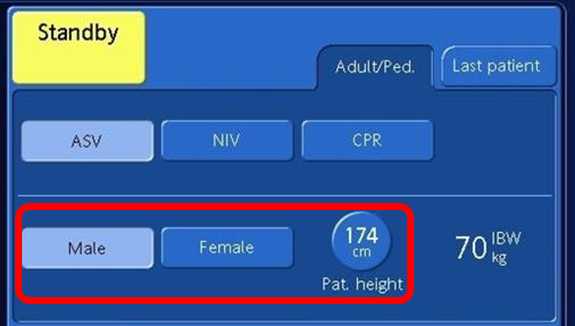
Step 1: Determine patient height and select gender
See Figure 1 above.
Step 2: Initial settings
Be aware that tidal volumes delivered by ASV can be limited by means of the pressure limitation (Pasvlimit) setting. Adjust the Pasvlimit according your Pplateau measurement results if needed. Normally a Pasvlimit ≤30 cmH2O is sufficient; in severe cases with low chest wall compliance or high airway resistance, a higher Pasvlimit up to 35 cmH2O might be needed. Verify your PEEP and Pasvlimit settings according to transpulmonary pressure measurement. Keep the driving pressure below 14 cmH20 (
Step 3: Adjust %MinVol and Pasvlimit
Increase or decrease the %MinVol to reach the target PaCO2 in passive patients. In spontaneously breathing patients, increase or decrease the %MinVol to change the level of pressure support.
Step 4: Consider an early recruitability assessment
An RCT (
Full citations below: (
For additional information on COVID-19:
WHO guidelines: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance
ESICM information: https://www.esicm.org/resources/coronavirus-public-health-emergency/
Current evidence about COVID-19: https://jamanetwork.com/journals/jama/pages/coronavirus-alert
Centers for Disease Control and Prevention, CDC: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html

In this article we outline the recommendations for the respiratory treatment of COVID-19 patients drawn from recent literature and guidelines issued by various organizations worldwide. They reflect the status as at the date of last change shown here.

This article gives you step-by-step instructions on how to set the ventilator when using the ventilation mode INTELLiVENT®-ASV® on ARDS patients.