Author: Jean-Michel Arnal, Intensivist, Hôpital Sainte Musse, Toulon, France
Date of first publication: 27.09.2021

Distal airway closure is a physiologic phenomenon that occurs during forced expiration in awake, spontaneously breathing patients and explains why we can’t completely empty our lungs. In patients under anesthesia, complete airway closure in the dependent part of the lung is common (
In ARDS patients, repeated closures of the airway with trapped gas have recently been described (
Complete airway closure has been reported in 22% of obese, sedated patients with a normal lung (
There are several consequences of complete airway closure. First, cyclic airway closure affects the ventilation/perfusion ratio, which in turn impairs oxygenation of the blood. Poorly ventilated areas may eventually collapse, particularly if they are ventilated with a high fraction of oxygen. The result is absorption atelectasis, which induces shunt, further impairs blood oxygenation, and decreases lung compliance. Second, the amount of static airway pressure measured at end-expiration does not reflect alveolar pressure, because the alveoli are no longer communicating with the proximal airway. An end-expiratory occlusion usually shows a shape suggesting intrinsic PEEP, which corresponds with the pressure gradient between the distal airways upstream from the airway closure and the proximal airways (
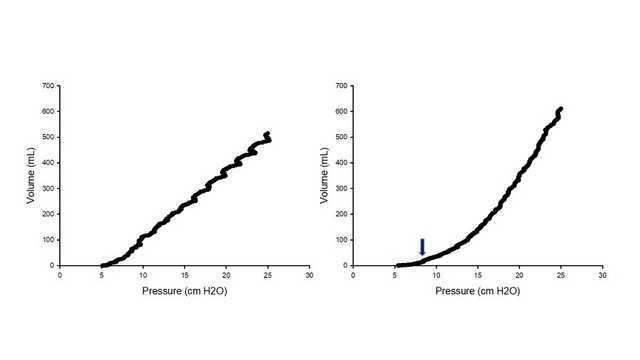
Airway closure is usually not detected during tidal ventilation, regardless of the ventilation mode used, and requires a low-flow inflation curve to be performed (see Figure 1). The initial part of the inflation shows either no or only a small volume increase because the airways are closed. Then, at a certain pressure corresponding to the AOP, inflation starts. This point has been wrongly interpreted as a low inflection point, intrinsic PEEP, or the pressure where regional transpulmonary pressure would become positive. AOP measurements report values of between 5 and 20 cmH2O (
Complete airway closure can be alleviated by using recruitment maneuvers and setting PEEP to a value greater than the AOP (
Using the P/V Tool® Pro on Hamilton Medical ventilators (