Autor: Clinical Experts Group, Hamilton Medical
Fecha: 30.09.2020
Last change: 30.09.2020
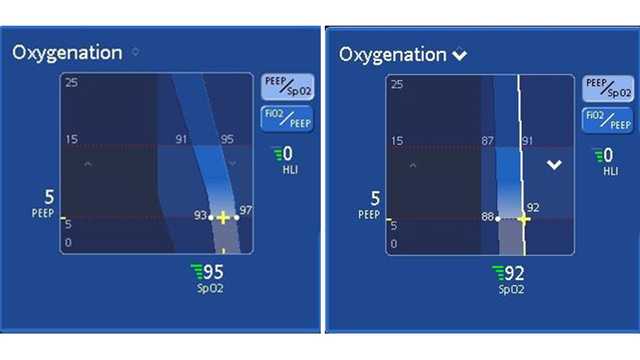
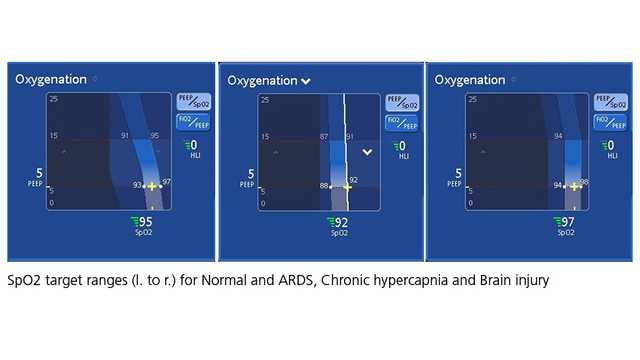
(Originally published 30.08.2017) Previously: chronic hypercapnia range 88-93%; brain injury range 96-99%. New screenshots.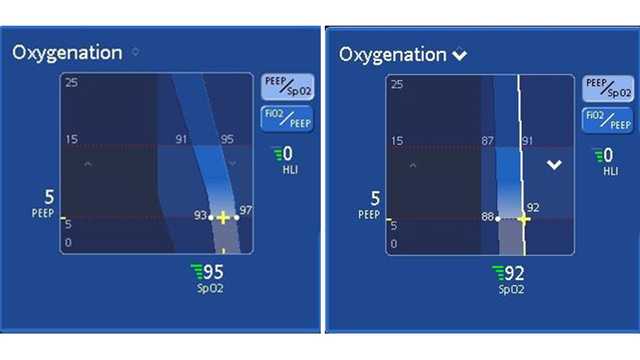
When using INTELLiVENT®-ASV® (
Full citations below: (