Autor: Süha Demirakca
Fecha: 19.12.2018
However, before starting any form of therapy, the top priority must be to reassure the child and ensure its wellbeing. Any child having difficulty breathing is usually very scared! It is therefore helpful to discuss the upcoming treatment measures with the child in a manner appropriate for the child’s age, and in the presence of the child’s parents. The following considerations are also important:
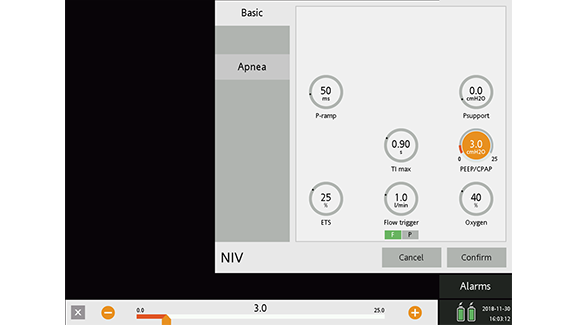
Start with PEEP of 4 cmH2O (less is also possible depending on how sensitive the child is). Gradually increase PEEP in steps of 1–2 cmH2O to familiarize the patient with the treatment, until you reach your targeted optimum for functional residual capacity (FRC).
Target parameters:
Maximum values: PEEP of greater than 8–10 cmH2O is usually not necessary and brings with it more drawbacks than benefits. If higher PEEP is necessary, you should intubate the patient.
This relieves the patient of much of the work of breathing and thus the dyspnea. Start the Psupport with 1–2 cmH2O and gradually increase it in steps of 1–2 cmH2O to familiarize the patient, until you can see clinically obvious relief from dyspnea and work of breathing.
Target parameters:
Maximum values: As a rule, no more than 10–12 cmH2O is necessary (see "Peak pressure“).
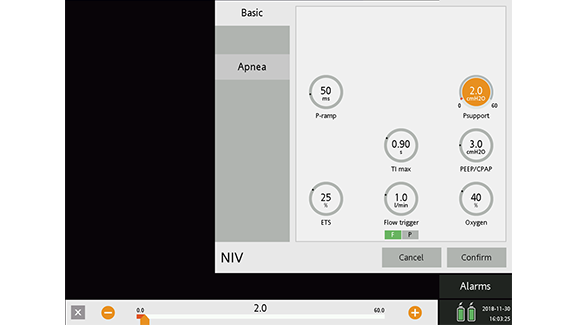
The peak pressure should not be more than 20–22 cmH2O. Firstly, this avoids exceeding the esophageal opening pressure which may lead to gastric overdistension. Secondly, it prevents transpulmonary pressures from rising to more than 30 cmH2O, which can significantly increase the risk of lung injury.
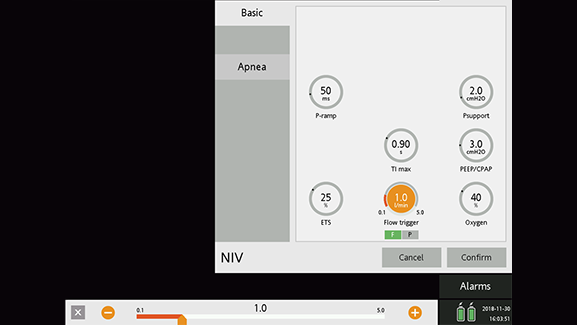
Start with 1 l/min, gradually increase or lower the trigger sensitivity in steps of 0.1 ml/min so that no autotriggering occurs and, at the same time, the incidence of ineffective efforts is as low as possible.
Target parameters:
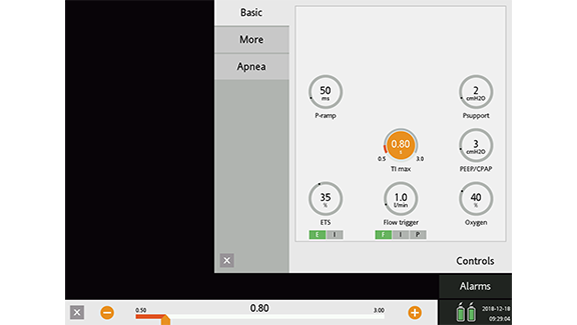
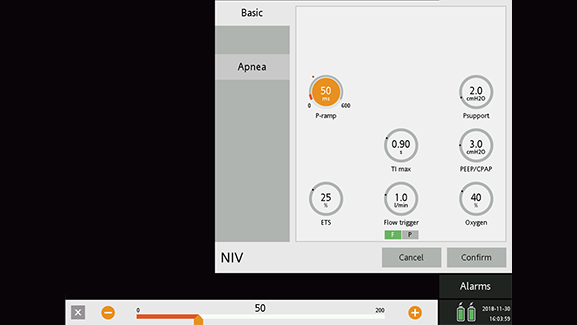
Start with 100 ms.
Target parameters:
The expiratory trigger sensitivity setting determines at what percentage of the peak inspiratory flow the breath is cycled off.
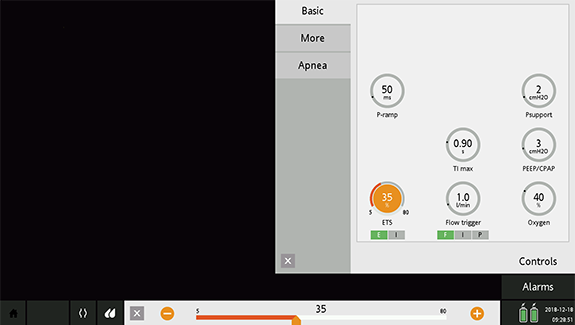
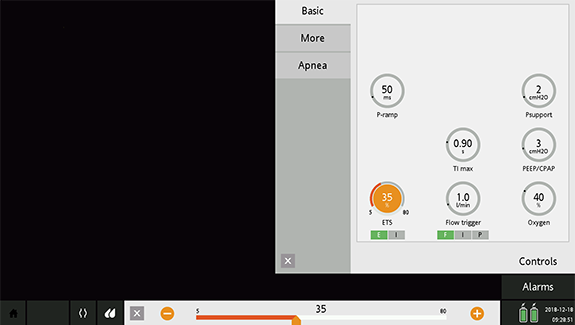
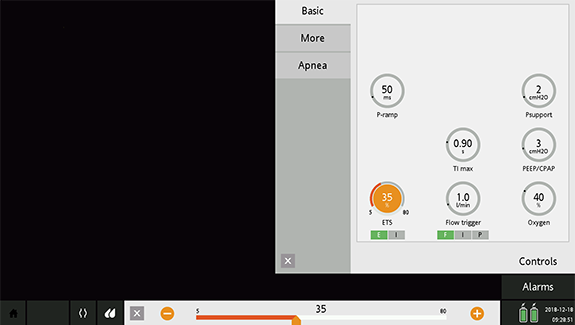
Start with ETS at 35%.
Target parameters:
Start with 125% of a TI suitable for the patient’s age.
After reaching a steady state, shorten the time to the minimum of TI max that can be tolerated.
Full citations below: (