El sensor de flujo proximal ha sido la piedra angular de nuestros respiradores desde 1983. Todo el proceso de ventilación depende de la medición y precisión del sensor de flujo, que proporciona datos procedentes de la apertura de las vías aéreas.
La obtención de datos de presión, flujo y volumen precisos es fundamental para emitir un diagnóstico correcto y evitar los efectos secundarios habituales consecuencia de la configuración incorrecta del respirador. También admite algunas de nuestra tecnologías avanzadas, como los modos ASV e INTELLiVENT-ASV, además de IntelliSync+ y P/V Tool.

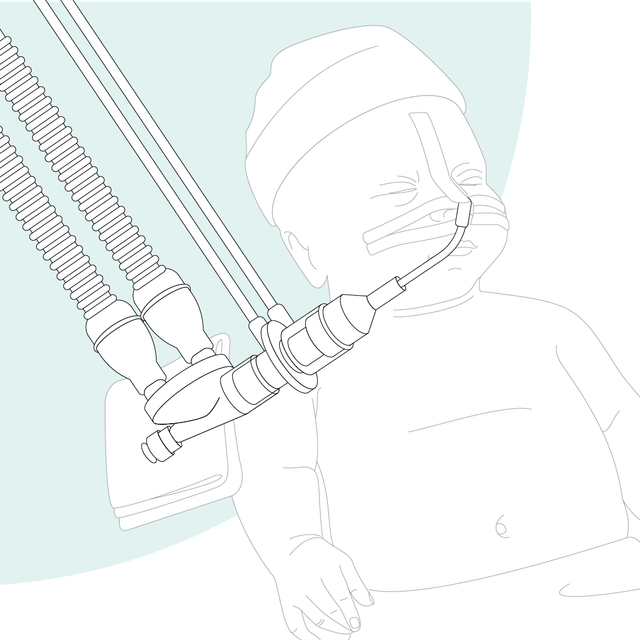
Nuestros respiradores miden el flujo y la presión cerca de la vía aérea del paciente. Los estudios han demostrado que los volúmenes tidales de los pacientes con ventilación se deben determinar con un sensor de flujo ubicado en el tubo endotraqueal (

La determinación precisa del volumen tidal espiratorio (VTE) es fundamental (
Beneficios para usted:
Ofrecemos material fungible de Hamilton Medical para pacientes adultos, pediátricos y neonatos. Puede elegir entre productos reutilizables o desechables, en función de las políticas de su centro sanitario.
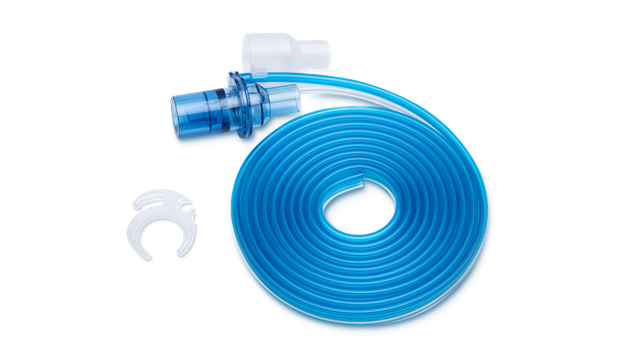

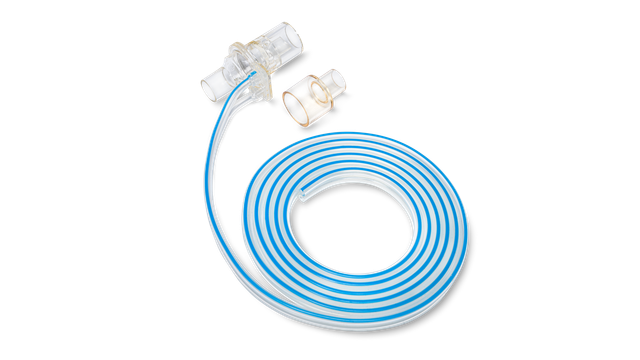

Los sensores de flujo desechables de Hamilton Medical ayudan a evitar la contaminación cruzada, ya que no hay que preocuparse de que vuelvan a utilizarse en otro paciente.
Director del departamento de Asistencia Respiratoria hasta 2018
University Medical Center, Lubbock (TX), EE. UU.