
Autor: Caroline Brown, Giorgio Iotti
Fecha: 08.07.2022
La presencia de asincronías entre el paciente y el respirador es una situación habitual en pacientes con ventilación mecánica (1, 2).

Este desfase entre los tiempos de inspiración y espiración del paciente y el respirador puede presentarse de distintas formas, es decir, puede provocar ciclos tempranos o tardíos, disparos automáticos o disparos dobles, o esfuerzos ineficaces, lo cual ha demostrado tener un impacto en los resultados de los pacientes (
El concepto de analizar las formas de onda de presión y flujo de las vías aéreas para detectar esfuerzos respiratorios y sus tiempos se describió por primera vez hace casi tres décadas (
Un elemento clave de este ensayo fue el uso de un método sistemático para analizar las formas de onda de presión y flujo de las vías aéreas, que comprendía cinco principios fisiológicos generales y un conjunto de reglas específicas definidas de antemano (“el método de análisis de formas de onda”). Se administró ventilación a todos los pacientes en modo de presión de soporte mediante la colocación de un catéter esofágico. El método se aplicó a las formas de onda de presión y flujo de las vías aéreas que se obtuvieron utilizando un sensor proximal, y se utilizó como referencia la presión esofágica (Pes). Para cada paciente, tres investigadores de un equipo de cuatro (tres médicos jefe y un residente) analizaron solo las formas de onda de flujo y presión, mientras que otro investigador analizó las formas de onda de flujo y presión, además del trazado de la curva de Pes. Las respiraciones se clasificaron como respiraciones «normalmente» asistidas, respiraciones con disparo automático, respiraciones con disparo doble o esfuerzos ineficaces. En el caso de las respiraciones normalmente asistidas, también se evaluaron asincronías menores (retraso del disparo, ciclo temprano y ciclo tardío).
El criterio principal de valoración fue el porcentaje de esfuerzos espontáneos detectados mediante el método de análisis de formas de onda. Entre los criterios de valoración secundarios se encontraba la concordancia entre los métodos de análisis de formas de onda y de referencia en la detección de asincronías mayores y menores, así como la concordancia entre evaluadores para el método de análisis de formas de onda.
Se registró un total de 4426 respiraciones. Según las mediciones de la Pes de referencia, el 77,8 % de estas se identificaron como respiraciones detectadas correctamente por el respirador, el 22,1 % como esfuerzos ineficaces y el 0,1 % como respiraciones con disparo automático. El método de análisis de formas de onda permitió detectar el 99,5 % de los esfuerzos espontáneos y todas menos una de las respiraciones con disparo automático. Del mismo modo, la concordancia entre los métodos de referencia y de análisis de formas de onda para identificar las respiraciones como asistidas, con disparo automático, con disparo doble o esfuerzos ineficaces fue muy alta. El índice de asincronía, calculado como la suma de las respiraciones con disparo automático, con disparo doble y esfuerzos ineficaces, dividido por el número total de respiraciones, fue del 5,9 % y no difirió cuando se evaluó mediante el método de análisis de formas de onda frente a la presión esofágica. El tiempo de asincronía total, calculado como el tiempo durante el cual el respirador y el paciente no están sincronizados, dividido por el tiempo total de registro, fue del 22,4 % y las asincronías menores representaron el 92,1 % del mismo. La concordancia entre los diferentes operadores para clasificar las respiraciones también fue muy alta.
En más del 90 % de los casos, el método de formas de onda permitió a los investigadores identificar el inicio y el final de los esfuerzos respiratorios con suficiente precisión como para identificar correctamente que las asincronías menores (retraso del disparo, ciclo temprano y ciclo tardío) también eran posibles.
Este estudio presenta algunos hallazgos importantes. Los investigadores demuestran que el método de análisis de formas de onda permite a los profesionales sanitarios detectar un porcentaje extremadamente alto de esfuerzos espontáneos y evaluar con precisión el tiempo de actividad del paciente. Incluso para asincronías menores, el método de análisis de formas de onda es altamente fiable y reproducible. La importancia de esto queda subrayada por otro hallazgo del estudio, es decir, que la mayor parte del tiempo de asincronía en PSV estuvo relacionado con asincronías menores.
Estos resultados, además de demostrar la reproducibilidad del método de análisis formas de onda (alta concordancia entre operadores), denotan la importancia fundamental de la formación en análisis de formas de onda de acuerdo con un método sistemático predefinido. Las pruebas han demostrado que la experiencia clínica en el tratamiento de pacientes con ventilación mecánica no proporciona necesariamente la competencia necesaria para el reconocimiento de asincronías, que en general es bastante baja en los médicos de la UCI (
Los autores concluyen asimismo que las formas de onda proximales de la presión y el flujo de aire de las vías aéreas aportan información suficiente para evaluar con precisión la actividad del paciente y la interacción entre el paciente y el respirador, siempre que se adopte un método de análisis sistemático adecuado como el “método de análisis de formas de onda”.
La tecnología IntelliSync®+ integrada en los respiradores de Hamilton Medical(
Puede consultar las citas completas a continuación: (

Nuestra hoja de referencia de asincronías incluye una descripción general de los tipos de asincronías más comunes, sus causas y cómo detectarlas.
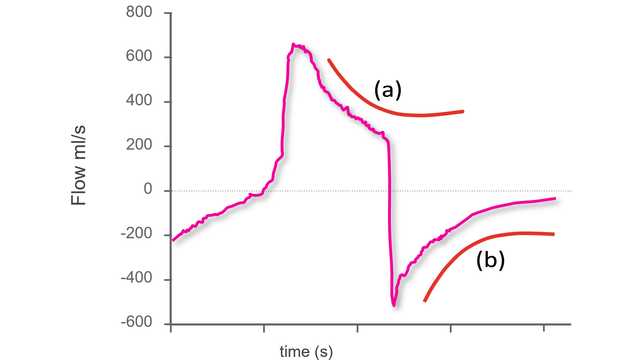
El primer paso para identificar asincronías mediante formas de onda de respiradores estándar consiste en saber qué aspecto tiene una respiración síncrona durante una ventilación en modo de presión de soporte.
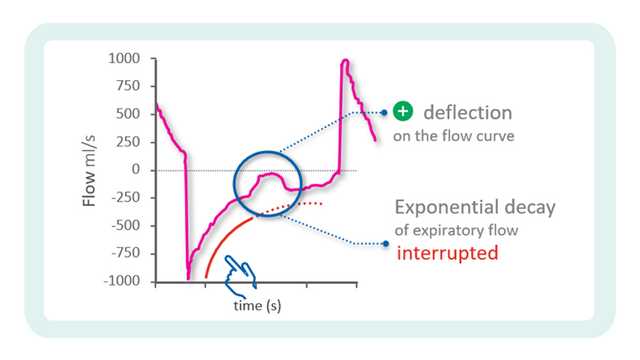
En nuestro consejo de cuidados a pie de cama del número anterior, explicamos el primer paso para identificar asincronías mediante el uso de formas de onda de respiradores.