
Auteur: Caroline Brown, Giorgio Iotti
Date: 08.07.2022
Les asynchronies entre le patient et le ventilateur sont fréquentes chez les patients ventilés mécaniquement (1, 2).

Ce décalage entre les temps inspiratoires et expiratoires du patient et le ventilateur peut prendre différentes formes, comme un cyclage précoce ou tardif, un déclenchement automatique, un déclenchement double ou des efforts inefficaces, et s'est avéré avoir un impact sur les résultats du patient (
Le concept visant à analyser les formes d'ondes de débit et de pression des voies aériennes pour détecter des efforts respiratoires et leur minutage a été décrit pour la première fois il y a presque trois décennies (
Un élément clé de cet essai a consisté à utiliser une méthode systématique visant à analyser les formes d'ondes de débit et de pression des voies aériennes, qui comprenait cinq principes physiologiques généraux et un ensemble de règles spécifiques définies au préalable (« Méthode de la forme d'ondes »). Tous les patients étaient ventilés en mode avec aide inspiratoire et avec un cathéter œsophagien en place. La méthode a été appliquée aux formes d'ondes de débit et de pression des voies aériennes obtenues à l'aide d'un capteur proximal, et la pression œsophagienne (Pes) a été utilisée comme référence. Pour chaque patient, trois chercheurs d'une équipe de quatre personnes (trois médecins-chefs et un interne) ont analysé les formes d'ondes de débit et de pression uniquement, tandis qu'un autre chercheur a analysé des formes d'ondes de débit et de pression, ainsi que le tracé de la Pes. Les cycles ont été répertoriés comme assistés « normalement », déclenchés automatiquement, à double déclenchement ou comme des efforts inefficaces. Dans le cas des cycles assistés normalement, des asynchronies mineures (retard de déclenchement, cyclage précoce et cyclage tardif) ont également été évaluées.
Le critère d'évaluation principal était le pourcentage d'efforts spontanés détectés à l'aide de la méthode de la forme d'ondes. Les critères d'évaluation secondaires comprenaient la concordance entre les méthodes de la forme d'ondes et de référence pour la détection d'asynchronies mineures et majeures, ainsi que le consensus entre les évaluateurs pour la méthode de la forme d'ondes.
Un total de 4 426 cycles ont été enregistrés. À l'aide des mesures de la Pes de référence, 77,8 % de ces cycles ont été identifiés comme des cycles correctement détectés par le ventilateur, 22,1 % comme des efforts inefficaces, et 0,1 % comme des cycles déclenchés automatiquement. La méthode de la forme d'ondes a permis de détecter 99,5 % des efforts spontanés et tous les cycles déclenchés automatiquement, sauf un. De même, la concordance entre les méthodes de référence et de formes d'ondes pour l'identification des cycles comme étant assistés, déclenchés automatiquement, à double déclenchement ou inefficaces était très élevée. L'indice d'asynchronie, calculé comme la somme des cycles déclenchés automatiquement, inefficaces et à déclenchement double, divisée par le nombre total de cycles, était de 5,9 % et n'a pas changé lors de l'évaluation à l'aide de la méthode de la forme d'ondes versus la pression œsophagienne. La durée totale d'asynchronie, calculée comme la durée pendant laquelle le ventilateur et le patient ne sont pas synchrones divisée par la durée totale d'enregistrement, était de 22,4 %, dont 92,1 % de ce chiffre représentaient des asynchronies mineures. Le consensus entre les différents utilisateurs en matière de classification des cycles était également très élevé.
Dans plus de 90 % des cas, la méthode de la forme d'ondes a permis aux chercheurs d'identifier le début et la fin des efforts respiratoires avec suffisamment de précision pour que l'identification correcte des asynchronies « mineures » - retard de déclenchement, cyclage précoce et cyclage tardif - soit également possible.
Cette étude présente quelques résultats importants. Les investigateurs montrent que la méthode de la forme d'ondes permet aux médecins de détecter un pourcentage extrêmement élevé d'efforts spontanés et d'évaluer précisément le minutage de l'activité du patient. Même dans le cas d'asynchronies mineures, la méthode de la forme d'ondes est très fiable et reproductible. L'importance de ce résultat est soulignée par un autre résultat de l'étude, à savoir que la majeure partie de la durée d'asynchronie en PSV était associée à des asynchronies mineures.
Ces résultats montrent non seulement la reproductibilité de la méthode de la forme d'ondes (consensus élevé entre les utilisateurs ) mais également que la formation à l'analyse des formes d'ondes suivant une méthode systématique prédéfinie joue un rôle clé. Les données ont montré que l'expérience clinique relative au traitement des patients ventilés mécaniquement n'implique pas nécessairement l'aptitude à reconnaître des asynchronies, qui est généralement assez faible chez les médecins USI (
Les auteurs ont conclu que les formes d'ondes proximales de débit et de pression des voies aériennes incluaient suffisamment d'informations pour évaluer précisément l'activité du patient et l'interaction patient-ventilateur, en supposant qu'une méthode d'analyse systématique appropriée telle que la « méthode de la forme d'ondes » soit adoptée.
La technologie IntelliSync®+ intégrée aux ventilateurs Hamilton Medical (
Citations complètes ci-dessous : (

Notre carte de référence des asynchronies fournit un aperçu des types d'asynchronies les plus courantes, leurs causes et comment les détecter.
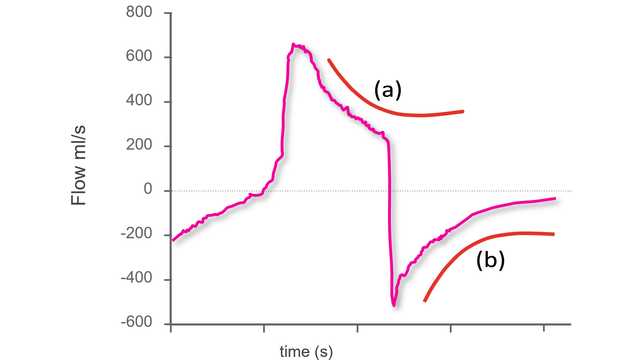
La première étape pour identifier des asynchronies à l'aide des formes d'ondes d'un ventilateur standard consiste à savoir à quoi ressemble un cycle synchrone pendant une ventilation avec aide inspiratoire.
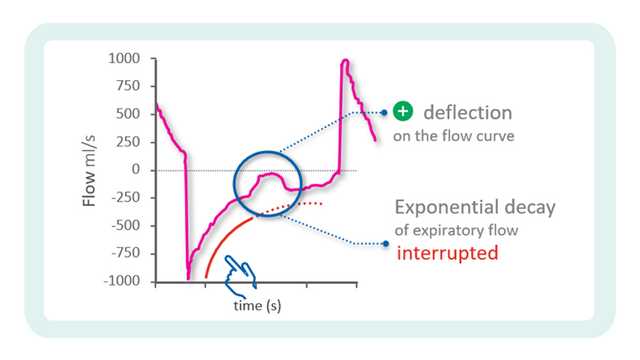
Dans la précédente partie, notre conseil pour une utilisation au chevet du patient traitait du point de départ pour l'identification des asynchronies à l'aide des formes d'ondes du ventilateur.