O sensor de fluxo proximal tem sido a peça central dos nossos respiradores desde 1983. Todo o processo de ventilação depende da medição e da precisão do sensor de fluxo, que fornece dados da abertura das vias respiratórias.
Dados precisos de volume, fluxo e pressão são cruciais para um diagnóstico correto e para evitar efeitos colaterais comuns de configurações inadequadas de ventilação. É também o que possibilita algumas de nossas tecnologias avançadas, como os modos ASV e INTELLiVENT-ASV, IntelliSync+ e a P/V Tool.

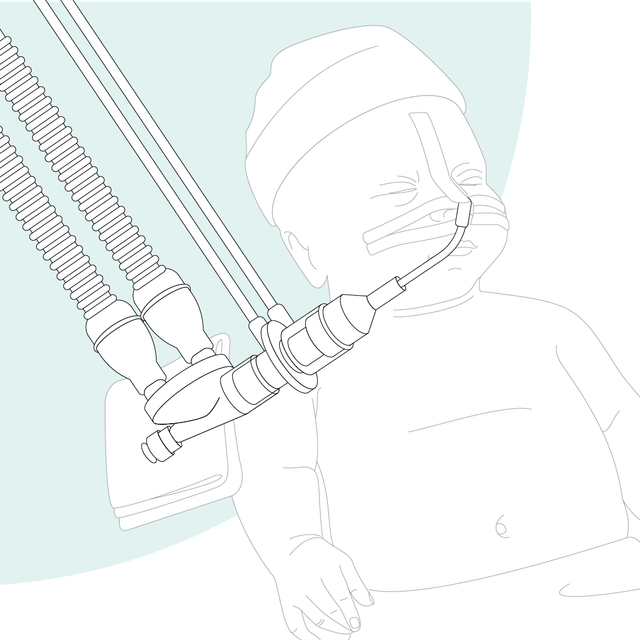
Nossos respiradores medem o fluxo e a pressão junto às vias aéreas do paciente. Estudos demonstraram que o volume corrente para pacientes ventilados deve ser determinado com um sensor de fluxo colocado no tubo endotraqueal (

É fundamental determinar com precisão o volume corrente exalado (VcorrExp) (
Benefícios para você:
Oferecemos consumíveis da Hamilton Medical para pacientes adultos, pediátricos e neonatais. Pode escolher entre produtos reutilizáveis e de uso único, dependendo das políticas da sua instituição.
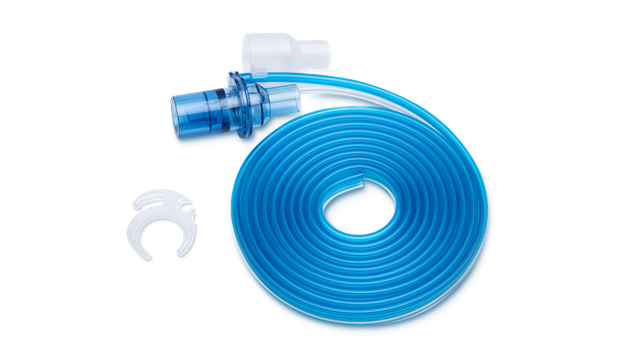

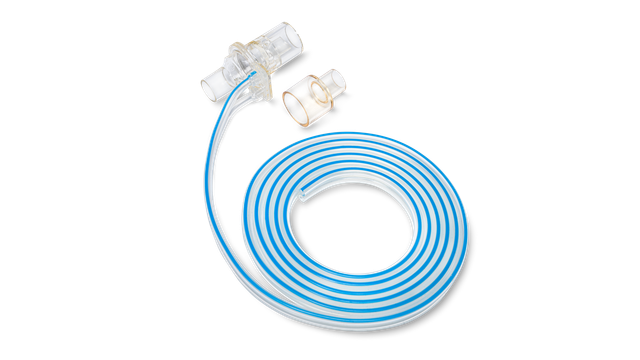

Os sensores de fluxo de uso único da Hamilton Medical nos ajudam a evitar a contaminação cruzada, pois não precisamos nos preocupar em reutilizar os sensores de fluxo em outro paciente.
Director of Respiratory Care até 2018
University Medical Center, Lubbock (TX), EUA