Фазы волюметрической капнограммы, форма и морфология кривой, а также измерения, основанные на ее расчетах, могут дать следующую важную информацию:
В наших аппаратах ИВЛ концентрация CO2 измеряется с помощью СО2-датчика для основного потока CAPNOSTAT-5, который находится рядом с дыхательными путями пациента.
Датчик CAPNOSTAT-5 обеспечивает точное измерение концентрации углекислого газа в конце выдоха (PetCO2), а также дает точную капнограмму при частоте дыхания до 150 дыхательных движений в минуту.
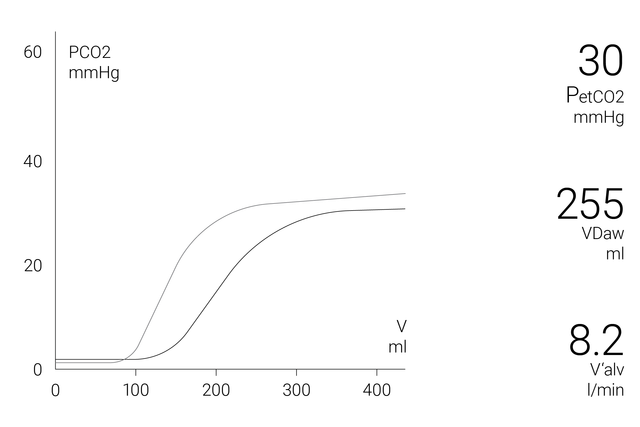
В окне волюметрической капнограммы на экране отображается точная количественная информация в виде комбинации данных проксимального потока и уровня CO2, таких как:
Для более полного анализа состояния пациента в аппаратах ИВЛ предусмотрена функция определения трендов за 72 часа (в аппаратах ИВЛ HAMILTON-G5/S1 – за 96 часов) для следующих параметров:
Для удобства пользователя в аппаратах ИВЛ Hamilton Medical все значения, связанные с CO2, отображаются в окне «Мониторинг CO2».
Узнайте, как читать волюметрические капнограммы, каковы их преимущества и где применять полученные данные. Книга также содержит тест для самопроверки.
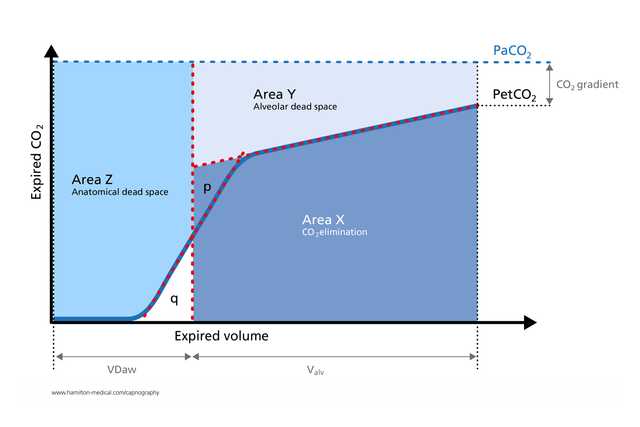
Волюметрическая капнограмма успешно используется для измерения анатомического мертвого пространства, перфузии легочных капилляров и эффективности вентиляции (
Расчеты, полученные с помощью волюметрической капнографии, используются для выявления эмболии сосудов легких у постели больного (
Исследование показало, что при волюметрической капнографии результаты измерения соотношения физиологической объемной части мертвого пространства и дыхательного объема у пациентов с ARDS, находящихся на искусственной вентиляции легких, отличаются такой же точностью, как и результаты, полученные методом метаболического мониторинга (
Экспираторная капнограмма – это быстрое неинвазивное измерение, не зависящее от дыхательного усилия, которое помогает выявить выраженный бронхоспазм у взрослых пациентов с астмой (
Волюметрическая капнография дает ценную информацию о физиологии коллапса легких и рекрутмента неинвазивным способом в реальном времени и таким образом позволяет контролировать цикличное выполнение маневров рекрутмента при лечении пациента (

Компания Hamilton Medical предлагает оригинальные расходные материалы для всех групп пациентов: взрослых, детей и младенцев. Доступны продукты для многократного или разового использования, (выбор зависит от политики вашего учреждения).
Волюметрическая капнография доступна как опция в аппаратах ИВЛ HAMILTON-C6, HAMILTON-G5, HAMILTON-C3 и HAMILTON-C1/T1, а также как стандартная функция в аппарате HAMILTON-S1.