
Esophageal pressure (Pes) measurement is a minimally invasive monitoring method, which enables us to determine the transpulmonary pressure.
The most common way to measure Pes is using an air-filled balloon integrated into an esophageal catheter.
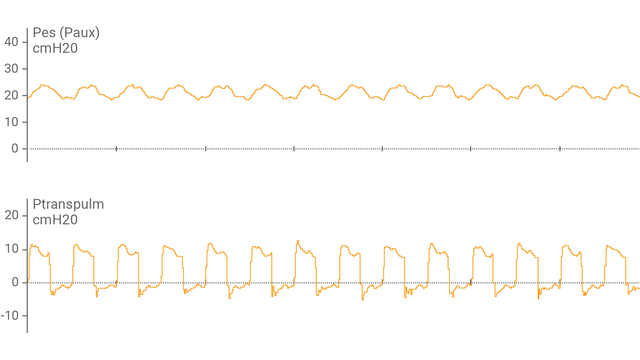
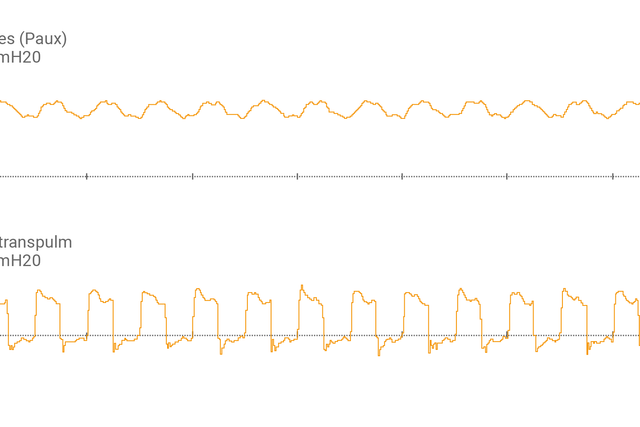
After you have connected the esophageal balloon catheter to the auxiliary port and confirmed the correct placement, the ventilator display shows esophageal pressure (Pes) and transpulmonary pressure (Ptranspulm) as a waveform.
You can measure static Ptranspulm using inspiratory and expiratory hold maneuvers.

For assessing recruitability and performing recruitment maneuvers, transpulmonary pressure can also be used in combination with the P/V Tool® Pro.
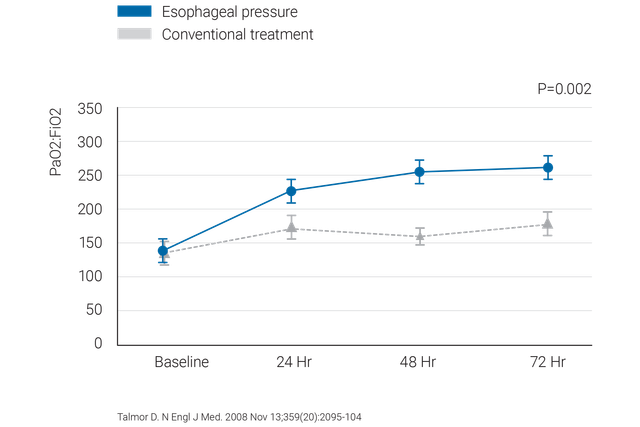


Clinically proven recommendations about what to do and what to avoid when using esophageal pressure in ARDS patients.
We offer esophageal ballon catheters from Cooper Surgical and naso-gastic catheters from NutriVent.
Transpulmonary pressure monitoring is a standard feature on the HAMILTON-C6.