Hamilton Medical 为HAMILT0N-C1/T1/MR1 呼吸机提供可选的说话阀功能。在压力控制模式自主呼吸(Spont)、压力控制通气(PCV+)和压力型同步间歇指令通气(P-SIMV+)下可以激活此功能。
使用说话阀功能的前提条件是:在气囊放气后上气道有足够的通畅性(开放性),并且有获批与呼吸机配合使用的说话阀,如Passy Muir 生产的PMV 007(湖绿色)(15 mm 内径/22 mm 外径)。PMV 即一个单向阀,只允许空气从呼吸机流向患者。由于在呼气过程中没有空气可以回流到呼吸机,因此当使用说话阀功能时,所有潮气量报警均基于吸气量。且分钟通气量和呼吸暂停报警被禁用。有关说话阀功能的一些常见问题,请参阅下面回答。
1. 压力和容量是测量值还是计算值?是否可以确定肺部 压力有多大?
(吸气)压力和流量在近心端流量传感器处测量。在有说话阀和没有说话阀的情况下, 显示值( 气道峰压 ( Ppeak ) 、平均气道压( Pmean ) 、呼气末正压 (PEEP);吸气时间(TI)、呼气时间(TE)、吸呼比 (I:E);吸入潮气量(VTI))与肺部压力的对应程度均相同。但是,呼吸机不能测量呼气值,因为PMV 在呼吸机方向处于关闭状态,空气只能通过上气道排出。
2. 当患者说话时,声带一张一合。呼吸机对此有何反应?
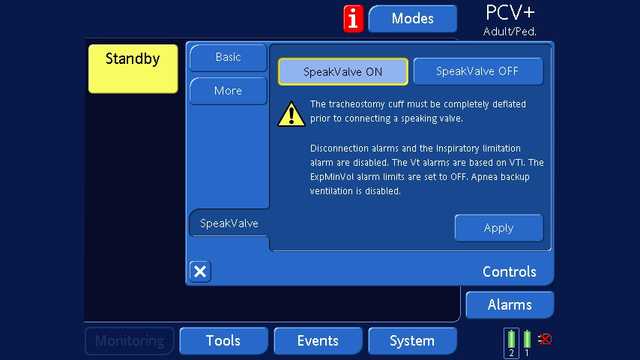
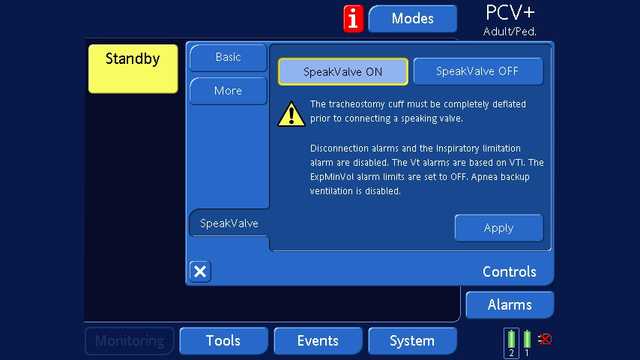
说话阀功能仅在压力控制模式下可用。因此,呼吸机需尝待机模式说话阀打开 说话阀关闭基本更多说话阀应用控制工具事件系统报警监测在连接说话阀之前,气管切开插管气囊必须完全放气。断开连接报警和吸气限值报警禁用。潮气量(Vt)报警基于吸入潮气量(VTI)。呼出分钟通气量(ExpMinVol)报警限值设置为“关闭”。窒息后备通气禁用。PCV+成人/儿童试达到设定压力。如果出现漏气,通过在呼吸期间增加流量给予补偿。
3. 当使用说话阀时,预计通过PEEP 保持开放的肺泡腔会完全塌陷吗?
事实证明并非如此。“在这组危重症通气患者中,在呼吸机撤机期间使用说话阀(SV)时不会导致肺不张。在使用说话阀期间和之后,对气管切开插管气囊进行放气并用单向阀恢复通过上气道的气流可以促进肺复张,这一点可通过呼气末肺阻抗(EELI)增加来表明(
4. 压力支持是否保持为设定值?
维持设定压力支持(Psupport)直至达到最大漏气补偿。
5. 空气陷闭的可靠指标是什么?
说话阀功能仅在压力控制模式下可用,因此呼吸机需尝试达到设定压力。如果由于气道阻塞或气管切开插管气囊意外充气导致空气不能通过上气道排出,肺部压力将不会增加到超过压力控制(Pcontrol)/Psupport 和PEEP 的总和。在下一次呼吸中,所应用的吸气量将急剧下降,因为肺部压力已达到目标值。因此,吸入潮气量(VTI)下降是表明空气陷闭发生的可靠指标。由于潮气量报警基于说话阀模式下的吸气量,因此可以识别到这种情况。