
食道压 (Pes) 测量是一种微创监测方法,我们可以通过它测定跨肺压。
最常用的 Pes 测量方法是使用与食道导管集成的气囊。
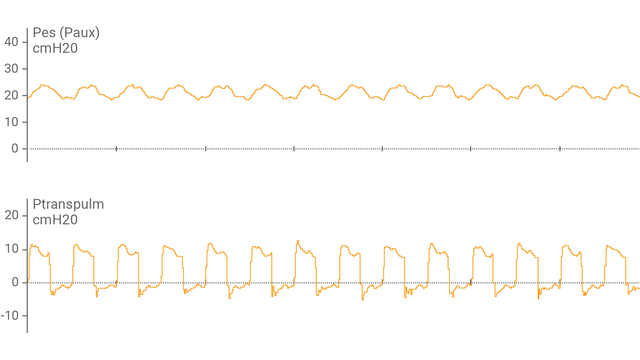
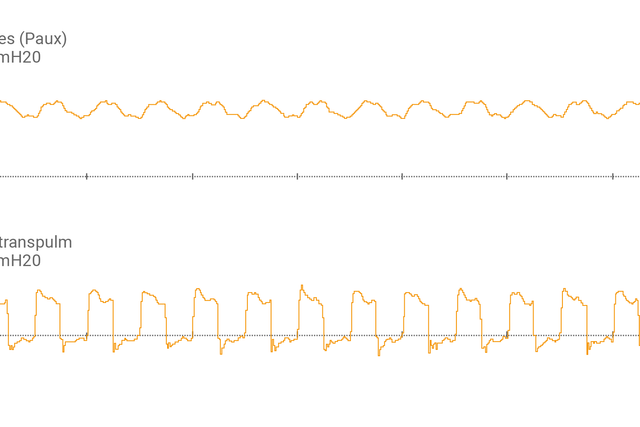
将食道气囊导管连接至辅助端口并确认正确放置后,呼吸机显示屏显示食道压 (Pes) 及跨肺压 (Ptranspulm) 波形。
您可以采用吸气和呼气屏气操作测量静态 Ptranspulm。

为了评估肺复张性和执行肺复张操作,跨肺压还可与 P/V Tool® Pro 配合使用。
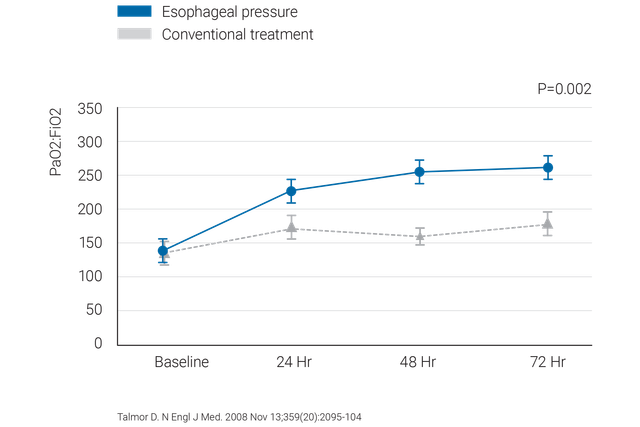


关于在 ARDS 病人中使用食道压力时应该做什么和应该避免什么的临床验证的建议。
我们提供 Cooper Surgical 食道气囊导管和 NutriVent 鼻饲管。
跨肺压监测是 HAMILTON-C6 呼吸机的一项标准功能。