脚注
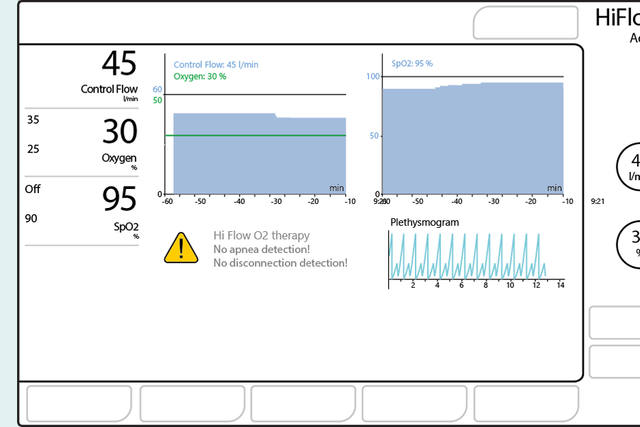
- A. 也称为高流量氧疗。此术语可与高流量鼻导管治疗互换使用。
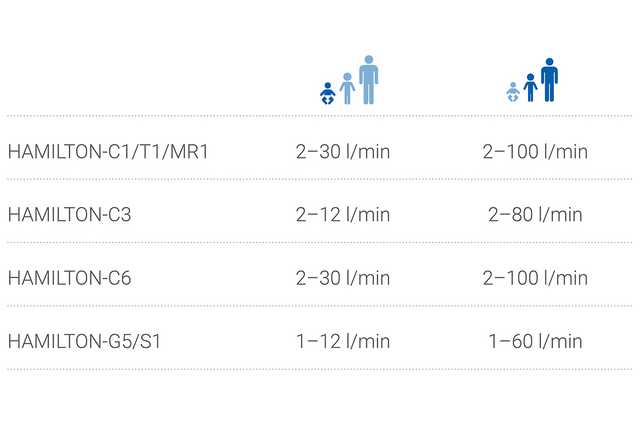
- B. 可以根据您的国家或设备要求改变流量。
参考文献
- 1. Frat JP, Thille AW, Mercat A, et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015;372(23):2185-2196. doi:10.1056/NEJMoa1503326
- 2. Delorme M, Bouchard PA, Simon M, Simard S, Lellouche F. Effects of High-Flow Nasal Cannula on the Work of Breathing in Patients Recovering From Acute Respiratory Failure. Crit Care Med. 2017;45(12):1981-1988. doi:10.1097/CCM.0000000000002693
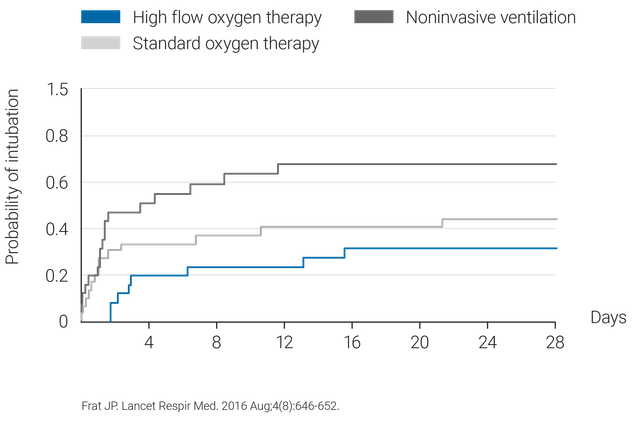
- 3. Frat JP, Ragot S, Girault C, et al. Effect of non-invasive oxygenation strategies in immunocompromised patients with severe acute respiratory failure: a post-hoc analysis of a randomised trial. Lancet Respir Med. 2016;4(8):646-652. doi:10.1016/S2213-2600(16)30093-5