Author: Caroline Brown, Branka Cupic
Date of first publication: 30.09.2022
In the previous issue, our Bedside tip covered the starting point for identifying asynchronies using ventilator waveforms.
The first step is to know what a normal breath looks like and how to recognize good synchrony between the patient and ventilator. We looked at the concept of exponential decay, and how to identify the start of an inspiratory effort and the well-synchronized end of inspiration.
The next step is how to identify the most common minor and major asynchronies.
Before looking more closely at those, we will recap the principles that formed the basis for a systematic method of waveform analysis applied by Mojoli et al. (
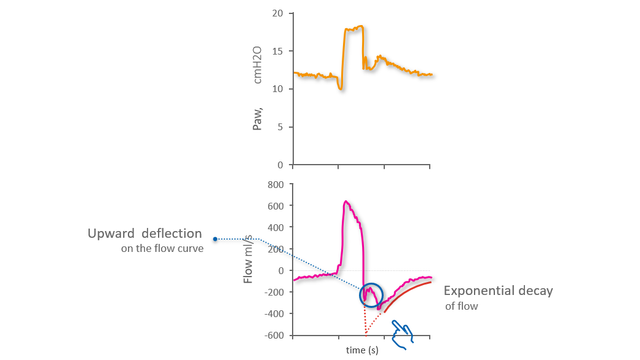
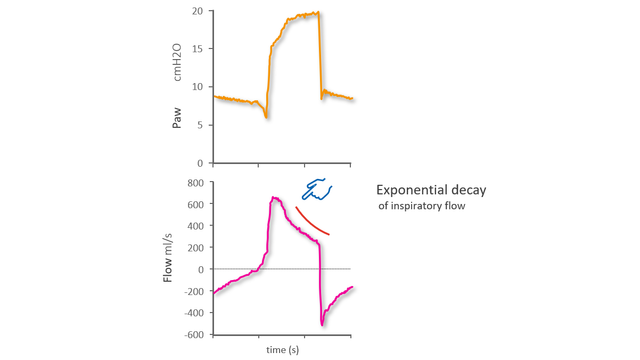
If patient and ventilator are synchronized and cycling is optimal, the Flow waveform will show the peak expiratory flow at the beginning of expiration, followed by exponential decay. Early cycling, whereby expiration starts before the inspiratory effort has ended, is denoted by a distortion of the initial expiratory flow: the normal peak flow is replaced by an upwards deflection, while the normal exponential decay starts later (see Figure 1 below).
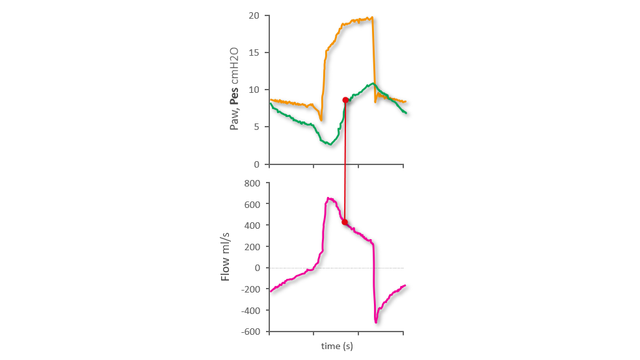
Using the esophageal pressure (Pes) waveform as a reference, we can see that the nadir of Pes (i.e., the point of maximum inspiratory effort) takes place during expiration and corresponds with the upwards deflection of the expiratory flow. The exponential flow decay starts later, namely at the end of the inspiratory effort as shown on the Pes waveform (see Figure 2 below). From our previous Bedside tip, we know that the fast increase in Pes after its nadir indicates relaxation of the inspiratory muscles, and the midpoint of this fast increase can be used as the reference for the end of inspiration.
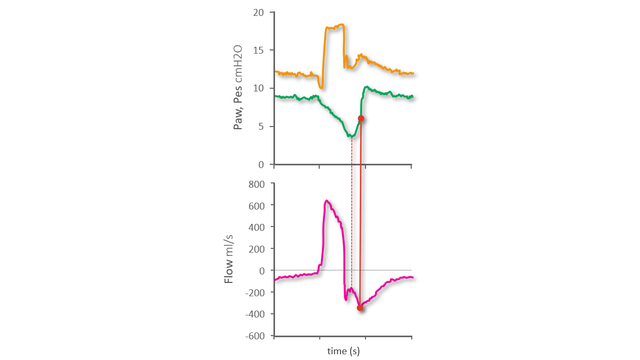
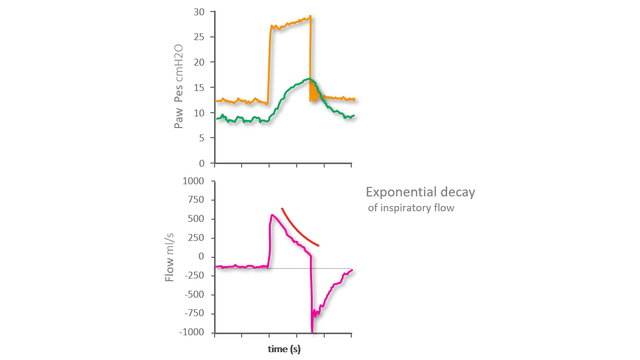
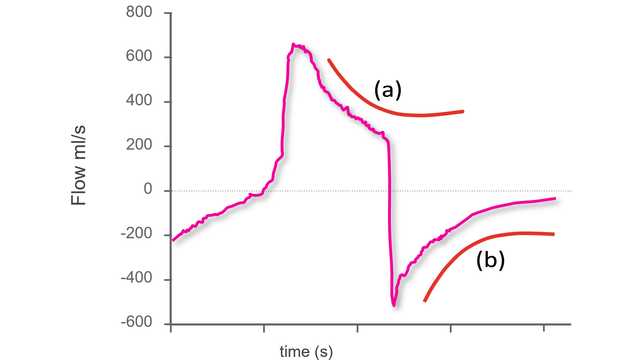
In the case of delayed cycling to expiration, there are two phases of inspiration. The first phase is caused by the normal synchronized pull of the inspiratory muscles and push from the ventilator, but inspiration then continues solely due to the push from the ventilator. This results in passive inflation. You can recognize this on the Flow waveform from the prolonged exponential decay of inspiratory flow occurring after the first phase with upwards convexity (see Figure 3 below).
On the Pes waveform we can see a point on the Pes rise after its nadir that marks a clear change of slope. This point corresponds with the transition from synchronized inspiration to the subsequent passive inflation caused by delayed cycling (see Figure 4 below).
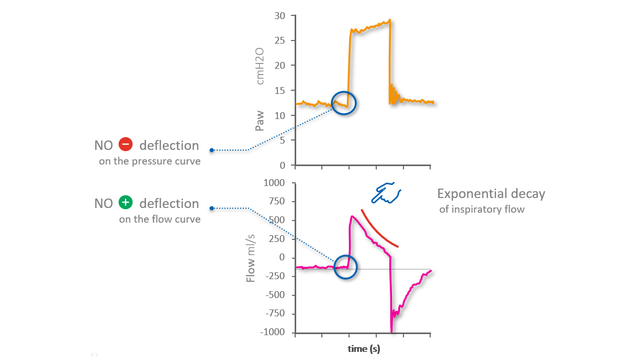
An auto-triggered breath is one triggered by the ventilator without an inspiratory effort made by the patient. Auto-triggering can be identified by watching both the Flow and Paw waveforms. There is no sign of the patient’s inspiratory effort, with neither a clear negative deflection of Paw, nor a clear positive deflection of Flow (with the exception of minimal oscillations due to cardiac activity (see Figure 5 below).
However, the strongest indication of auto-triggering can be seen on the inspiratory Flow waveform, which shows a very early peak followed by exponential decay: The whole inspiration is due to passive inflation. The shape of the peak itself is also an indicator: in the case of passive inspiration, the peak is a spike, whereas during synchronized inspiration it is more curved.
As on the Flow and Paw waveforms, there is no negative deflection visible on the Pes reference waveform that would normally indicate the start of the inspiratory effort (see Figure 6 below).
An ineffective inspiratory effort is an inspiratory effort made by the patient during the ventilator’s expiratory phase and not recognized – and therefore not supported - by the ventilator.
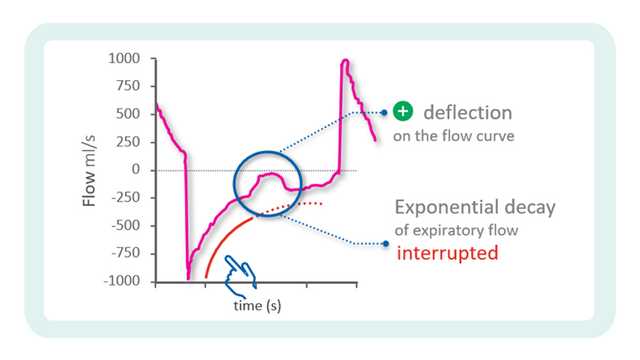
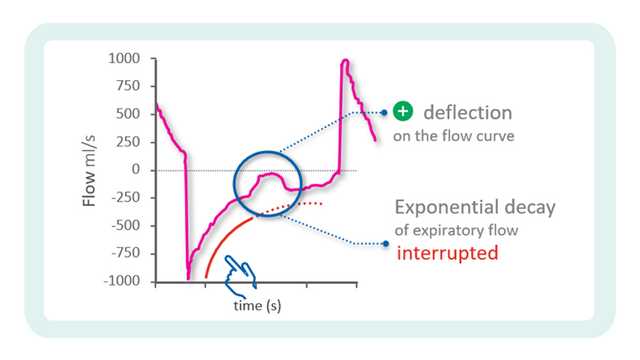
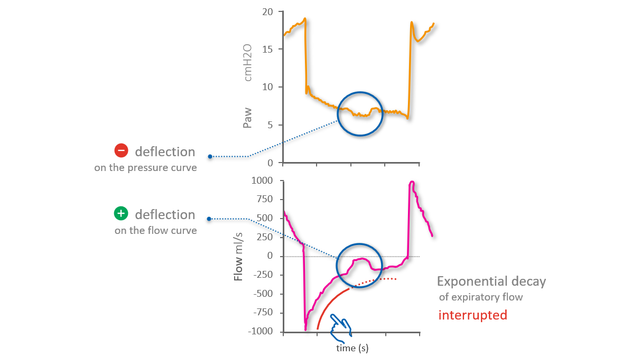
On the Flow waveform, you can identify the ineffective effort as a positive deflection temporarily interrupting the normal exponential decay of flow. On the Paw waveform, a minimal negative deflection occurs simultaneously (see Figure 7 below).
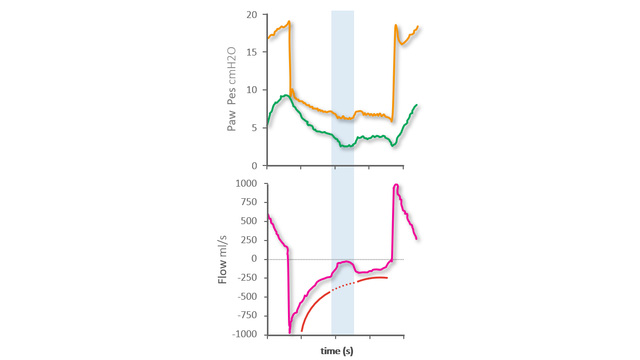
On the Pes reference waveform, you can see the beginning and end of the ineffective inspiratory effort shown as a negative deflection of Pes interrupting the normal expiratory decrease in Pes (see Figure 8 below).

Our asynchrony reference card gives you an overview of the most common asynchrony types, their causes, and how to detect them.
The first step to identifying asynchronies using standard ventilator waveforms is knowing what a synchronous breath looks like during pressure-support ventilation.

Asynchrony between patient and ventilator is a common occurrence in mechanically ventilated patients (1, 2).