Does the Hamilton Medical P/V Tool provide a real low-flow pressure/volume (P/V) loop?
The Hamilton Medical P/V Tool is a pressure-targeted method for producing a quasi-static P/V loop.
Flows of less than or equal to 10 l/min seem to be quick, safe, and reliable for determining the lung mechanics by means of a P/V loop at the bedside.
We suggest using the minimum ramp speed of 2 cmH2O/s to eliminate the pressure change from resistive elements of the respiratory system (
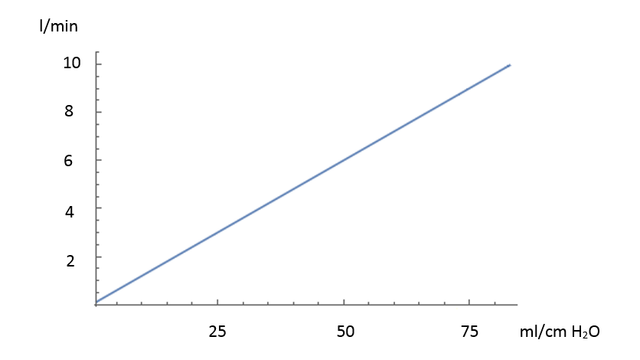
When following these recommendations, the flow should be below 10 l/min up to a compliance of 75 ml/cm H2O (see Figure 1). Most patients assessed for lung recruitability have a respiratory system compliance of less than 75 ml/cmH2O.
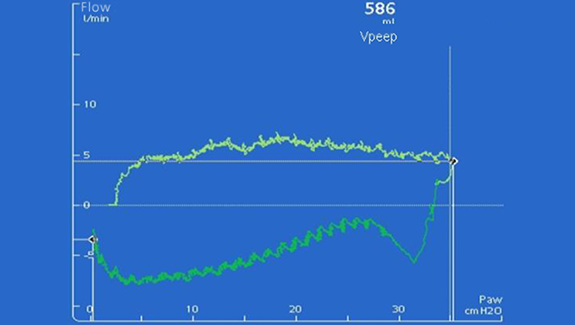
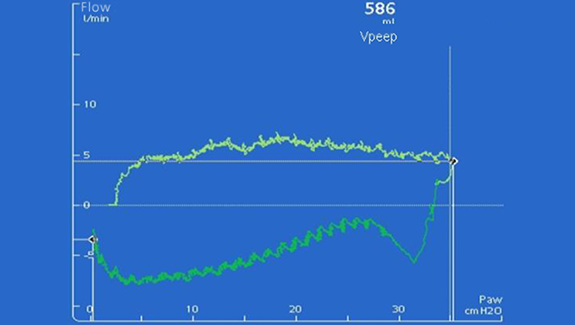
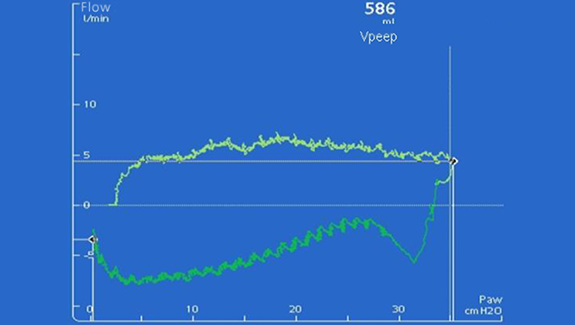
The flow can also be visualized by adding a Paw/Flow plot to the screen (see Figure 2).
It is not possible to have control of the expiratory flow, because it is driven by the elastic recoil of the respiratory system. Deriving the deflation limb by means of a pressure-control approach is a reliable method that shows a good correlation with the radiological findings of a CT-scan (
With the P/V Tool on selected ventilators (
Relevant devices: HAMILTON-G5/S1 (sw v2.8x), HAMILTON-C3 (sw v2.0.x), HAMILTON-C6 (sw v1.1.x)