Author: Hamilton Medical
Date of first publication: 11.09.2017
Last change: 28.07.2023
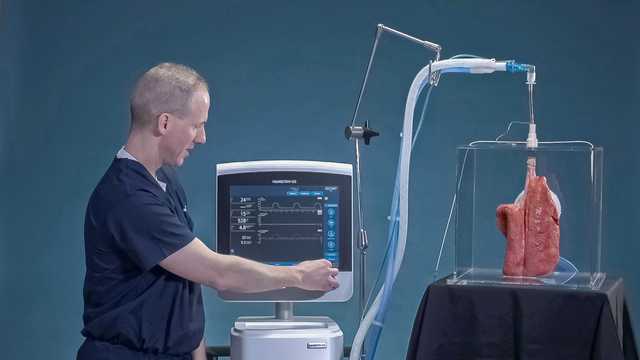
Transpulmonary pressure measurement changed to monitoringOne of the greatest challenges when mechanically ventilating patients is finding the correct setting for positive end-expiratory pressure (PEEP). This task can be made easier by using transpulmonary pressure monitoring to distinguish between the pressure in the lungs and the chest wall components.
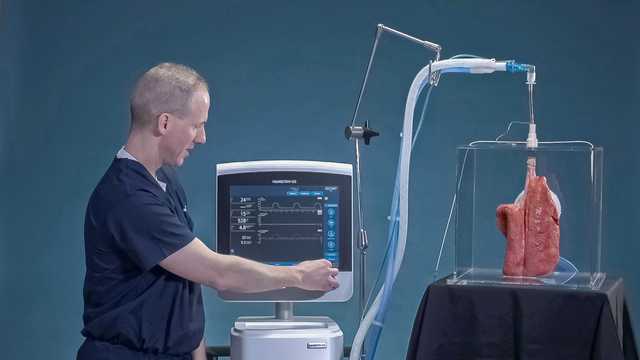
The ability to partition between the lung and chest wall components helps you to set the optimal PEEP, define a safe range for driving and plateau pressures, and to titrate and optimize lung recruitment maneuvers. But how can you distinguish between them when the pressures measured at the airway opening cannot be used to accurately assess the stress and strain applied to the lungs? A simple way of partitioning them is by using esophageal pressure measurement. The airway pressure minus the esophageal pressure measured during an end-inspiratory or an end-expiratory occlusion gives you the transpulmonary pressure, which represents the true distending pressure of the lungs.
Transpulmonary pressure monitoring is available on the HAMILTON-G5/S1 (
In patients with acute respiratory distress syndrome (ARDS), you can set PEEP in order to achieve a transpulmonary pressure of 0 to 5 cmH2O at end expiration, with the aim of preventing atelectrauma caused by repeated opening and closing of the distal airways and alveoli. Transpulmonary pressure monitoring can also be used to set the tidal volume and inspiratory pressure for ARDS patients, and together with the P/V Tool® to assess lung recruitability and perform recruitment maneuvers.
The video below shows you how to set PEEP using transpulmonary pressure monitoring on a HAMILTON-G5 ventilator.

Transpulmonary pressure monitoring enables optimization of PEEP, tidal volume, and inspiratory pressure (