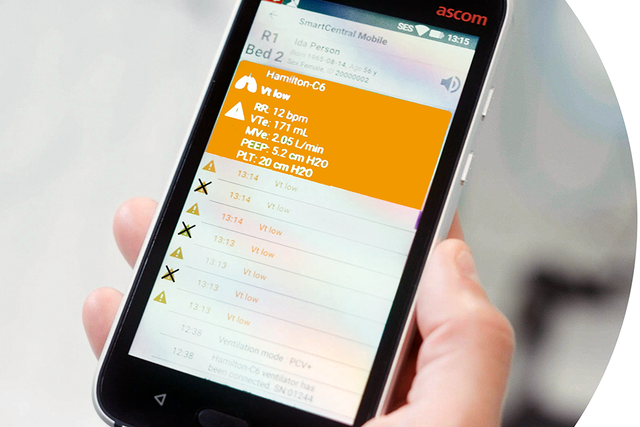
Il numero medio di allarmi per ogni paziente in terapia intensiva può superare i 700 al giorno. Si stima che una percentuale di questi allarmi compresa fra l'80% e il 95% non sia clinicamente significativa (, ).
L'esposizione a un tale numero di allarmi che non richiedono di intervenire può rappresentare una fonte di stress per il personale sanitario (). Questa situazione può a sua volta aumentare il rischio di danni ai pazienti e diminuire il livello di soddisfazione sia per i pazienti, sia per il personale medico (, ).