
Author: Matthias Himmelstoss
Date of first publication: 07.04.2020
Last change: 07.04.2020
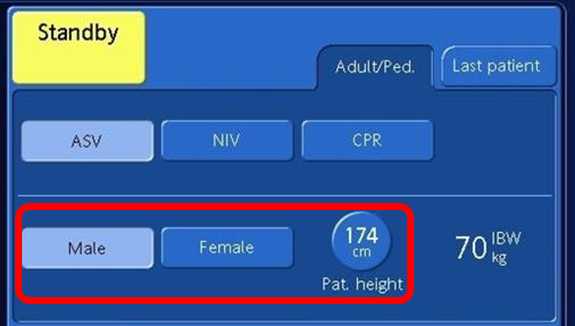
Addition of imagesThis article gives you step-by-step instructions on how to set the ventilator when using the ventilation mode INTELLiVENT®-ASV® on ARDS patients.

For additional information on COVID-19:
WHO guidelines: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance
ESICM information: https://www.esicm.org/resources/coronavirus-public-health-emergency/
Current evidence about COVID-19: https://jamanetwork.com/journals/jama/pages/coronavirus-alert
Centers for Disease Control and Prevention, CDC: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html