O olho treinado de um especialista em ventilação é capaz de detectar assincronias analisando as formas das ondas de fluxo e pressão.
No entanto, a condição do paciente pode mudar a cada respiração e o especialista não pode estar sempre junto ao leito.
É aí que o IntelliSync+ entra em ação. Esta tecnologia simula o olho do especialista para identificar o esforço (início da incursão) ou o relaxamento (início da excursão) do paciente na forma de onda
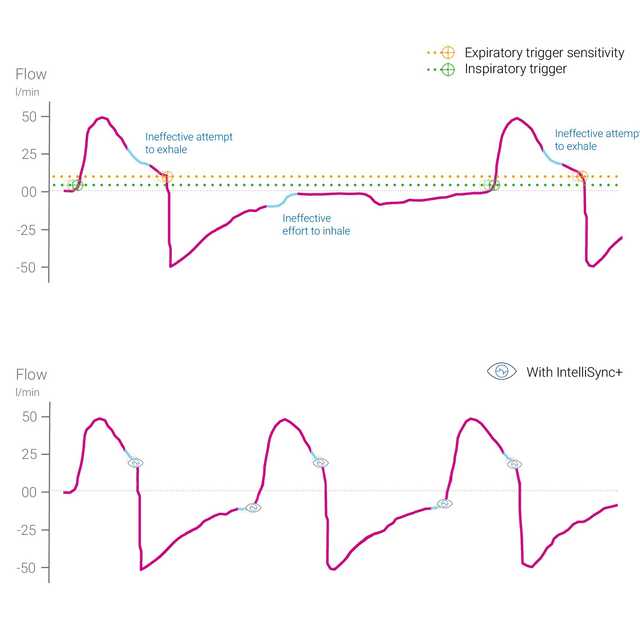
O IntelliSync+ analisa continuamente os sinais da forma de onda, pelo menos, cem vezes por segundo. Isso permite que o IntelliSync+ detecte imediatamente os esforços do paciente e inicie a inspiração e a expiração em tempo real substituindo assim as configurações convencionais de disparo para inspiração e expiração.
Para obter o máximo de flexibilidade, pode optar por ativar o IntelliSync+ para o disparo inspiratório, ou para o disparo expiratório, ou para ambos.

Um número elevado de assincronias graves entre o paciente e o respirador ocorre em cerca de 25% de todos os pacientes mecanicamente ventilados (
A análise das formas de onda é um método confiável, preciso e reproduzível para avaliar a interação paciente-respirador. A automação deste método pode permitir a monitorização contínua de pacientes ventilados e/ou melhorar o acionamento da respiração e o ciclo respiratório (
Mojoli F, Orlando A, Bianchi IM, et al.
Um estudo recente mostrou que o controle automatizado do ciclo de desligamento do respirador com base na análise em tempo real das formas de onda proporcionou um meio confiável de melhorar a sincronização em pacientes ventilados mecanicamente.


O IntelliSync+ é um método totalmente não invasivo que não requer qualquer hardware ou acessórios adicionais. Basta ativar a opção no seu respirador para utilizá-lo nos modos de ventilação invasiva ou não invasiva em pacientes adultos e pediátricos.
Como o IntelliSync+ também pode ser combinado com disparos convencionais, pode optar por utilizar o IntelliSync+ durante a inspiração, a expiração ou ambas.
O vídeo abaixo demonstra o IntelliSync+ em um HAMILTON-G5. O recurso funciona de forma semelhante em todos os dispositivos.


Nosso cartão de referência de assincronia oferece uma visão geral dos tipos de assincronia mais comuns, suas causas e como detectá-los.
IntelliSync+ está disponível como opção no HAMILTON-C6, no novo HAMILTON-C6, HAMILTON-C1, HAMILTON-T1, HAMILTON-MR1 e HAMILTON-G5, e é um recurso padrão no HAMILTON-S1.