As fases, a forma e a morfologia da curva de um capnograma volumétrico, assim como as medições derivadas dos cálculos, podem fornecer informações importantes sobre:
Nos nossos respiradores, o CO2 é medido com um sensor CO2 de fluxo direto CAPNOSTAT-5 junto das vias aéreas do paciente.
O sensor CAPNOSTAT-5 fornece medições precisas do dióxido de carbono ao final da expiração (PetCO2) e um capnograma claro e preciso em todas as frequências respiratórias até 150 respirações por minuto.
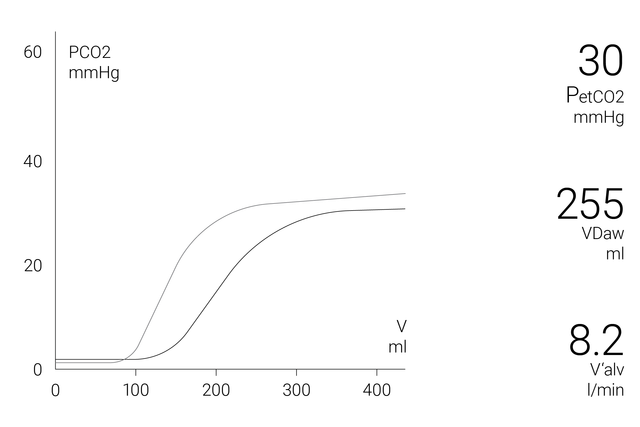
A janela do capnograma volumétrico na tela exibe informações quantitativas exatas, combinando dados de fluxo proximal e CO2 proximal, tais como:
Para permitir uma análise mais abrangente da condição do paciente, está disponível uma tendência de 72 horas (ou 96 horas com HAMILTON-G5/S1) para:
Para facilitar sua vida, os respiradores da Hamilton Medical oferecem uma visão geral de todos os valores relevantes relacionados ao CO2 na janela Monitorização de CO2.
Saiba como interpretar um capnograma volumétrico e obtenha uma visão geral dos benefícios e das aplicações clínicas da capnografia volumétrica. Inclui um autoteste!
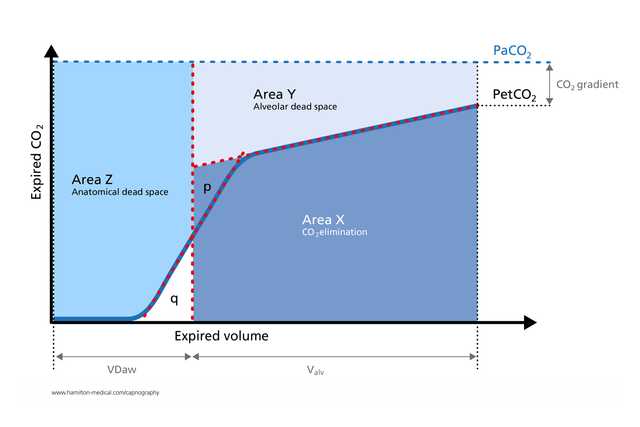
O capnograma volumétrico tem sido utilizado com sucesso para medir o espaço morto anatômico, a perfusão capilar pulmonar e a eficiência ventilatória (
Os cálculos derivados da capnografia volumétrica são úteis para identificar o embolismo pulmonar junto ao leito (
Em um estudo com pacientes com SARA submetidos à ventilação mecânica, as medições da capnografia volumétrica da relação fisiológica entre espaço morto e volume corrente foram tão precisas quanto as obtidas pela técnica de monitorização metabólica (
O capnograma expiratório é uma medição independente do esforço, rápida e não invasiva que pode ajudar a detectar broncoespasmos significativos em pacientes adultos com asma (
Ao fornecer informações importantes em tempo real sobre a fisiologia do colapso pulmonar e do recrutamento de forma não invasiva, a capnografia volumétrica é ideal para monitorar manobras de recrutamento cíclicas junto ao leito (

Oferecemos consumíveis originais para pacientes adultos, pediátricos e neonatais. Você pode escolher entre produtos reutilizáveis e de uso único, de acordo com as políticas institucionais.
A capnografia volumétrica está disponível como opção no HAMILTON-C6, no novo HAMILTON-C6, no HAMILTON-C3 e no HAMILTON-C1/T1.