
Author: Aude Garnero, Intensivist, Hôpital Sainte Musse, Toulon, France
Date of first publication: 04.05.2021
High-flow therapy (HFT) is a non-invasive form of respiratory support that can lower the intubation rate and mortality in patients with acute hypoxemic respiratory failure (AHRF) (1). Driven by concerns about the exposure of healthcare workers, initial recommendations discouraged the use of HFT in COVID-19 patients (2, 3).

However, due to the high morbidity and mortality resulting from early invasive mechanical ventilation (
The physiologic effects of HFT in acute hypoxemic respiratory failure are well-established, but there is no physiologic data specifically for COVID-19 pneumonia (
The washout of physiologic dead space by flushing expired air from the upper airway during expiration improves ventilatory efficiency. HFT reduces the minute ventilation needed to obtain a physiologic arterial CO2 level by decreasing the respiratory rate and anatomical dead space. Therefore, the alveolar ventilation (minute ventilation minus dead-space ventilation) remains stable, whereas the minute ventilation decreases. HFT also reduces the patient’s inspiratory effort and lessens the metabolic work of breathing. Finally, HFT improves respiratory mechanics, i.e., dynamic compliance, transpulmonary pressure, and ventilation homogeneity, and enhances patient comfort and tolerance when compared with conventional oxygen.
In a retrospective observational study (
A multicenter cohort study (
These two studies suggest that COVID-19 patients may benefit from HFT by decreasing the need for mechanical ventilation and its duration, as well as decreasing the ICU length of stay without having a negative impact on hospital mortality. However, there are no randomized controlled trials comparing outcomes in HFT patients with conventional oxygen or early intubation.
Three observational studies provide data from COVID-19 patients treated with HFT. Intubation rates were between 36% (
Data has shown that patients in whom HFT succeeded had a lower respiratory rate after HFT initiation than those patients who subsequently needed intubation (
The ROX (Respiratory rate-OXygenation) index is calculated from the respiratory variables that assess respiratory failure and can thus be used to predict the need for invasive ventilation. It represents the ratio of SpO2/FIO2 to RR. In acute hypoxemic respiratory failure due to non-COVID-19 pneumonia, the ROX index identified patients at low risk of HFT failure with a cut-off value of 4.88 measured after 12 hours of HFT (
The majority of studies on HFT in COVID-19 are either experimental or carried out on healthy subjects and therefore do not reflect real life. The World Health Organization commissioned reviews to examine the evidence on the use of HFT: Six simulation studies and one crossover study on non-COVID-19 patients were analyzed; HFT did not increase the risk of aerosol dispersion in comparison to typical patient breathing with violent exhalation; aerosol production levels and particle number concentrations found with HFT were similar to those with nasal prongs, non-rebreather masks, and spontaneous breathing (
Half of the environmental swab samples taken from the isolation room of a COVID-19 patient receiving HFT and non-invasive ventilation (NIV) showed positive results. However, all air samples were negative. Viable viruses were identified on one quarter of the sites. These findings highlight the need for use of personal protective equipment (
The incidence of COVID-19 infections before and after the implementation of HFT/NIV was measured in a US hospital. Results showed that use of HFT in a COVID-19 patient, when associated with the use of appropriate personal protective equipment and cohorting precautions, did not lead to a measurable increase in COVID-19 infections in healthcare workers (
Awake PP may improve the mismatch of ventilation-perfusion and open the atelectatic lungs by means of adequate sputum drainage. Two descriptive studies reported data from COVID-19 patients treated with HFT combined with PP. In the study of 10 patients (
In a prospective multicenter, adjusted cohort study (
HFT has been used in COVID-19 pneumonia related AHRF with favorable effects on oxygenation. Those patients who failed with HFT had a higher mortality rate because they were sicker at baseline. The ROX index may be used as a predictor of intubation, but the optimal cut-off is open to debate. If used with the appropriate protective equipment and precautions, HFT was shown not to increase contamination or infection of healthcare workers. The combination of HFT and PP requires further investigation.
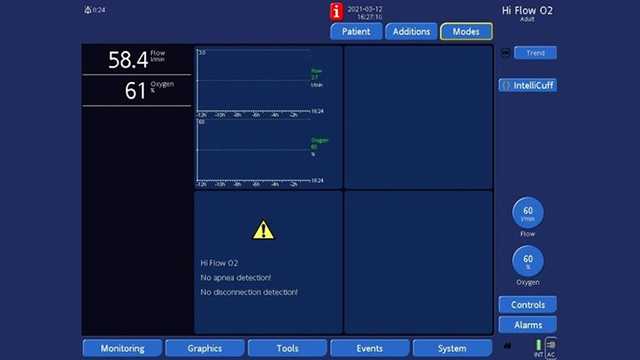
Ventilators from Hamilton Medical offer high flow oxygen therapy as a standard or optional feature, in addition to continuous SpO2 and SpO2/FiO2 measurement (
It is also available on our standalone high flow oxygen therapy device, the HAMILTON-HF90 (

Full citations below: (
Our e-book on high flow nasal cannula therapy gives you an overview of the working principles and clinical benefits, as well as practical information about choosing the right interface, adjusting the settings, and monitoring your patients.

Everything healthcare professionals need to know to get started with high flow nasal cannula therapy: the flow rate, FiO2 settings, when to use HFNC, selecting the interface, and much more.
High flow therapy (HFT) has been used widely during the COVID-19 pandemic. Published clinical experience is based mainly on retrospective studies and describes the main settings and the failure rate.
Learn everything you need to know in our guide to volumetric capnography: the volumetric capnogram, the capnography phases, what is dead space, the difference between anatomical dead space and alveolar dead space, PetCO during bronchospasm, V‘CO and CO2 elimination, and more.

The coronavirus pandemic has stretched many hospitals’ resources to the limit. Patients are requiring respiratory support on an unprecedented scale and a possible – or in some cases very real – shortage of ventilators is forcing institutions to weigh up the risks and benefits of alternative forms of therapy.