
Les solutions classiques de gestion de pression du ballonnet exigent de surveiller et d'ajuster manuellement la pression du ballonnet.
Vous pourriez nécessiter jusqu'à huit réglages manuels par jour pour maintenir en continu la pression du ballonnet dans les plages souhaitées (

Le dispositif IntelliCuff sécurise les voies aériennes de votre patient (
Vous pouvez l'utiliser soit comme un dispositif autonome pour tous les ventilateurs mécaniques, soit en tant que solution intégrée pour le HAMILTON-C6 et le HAMILTON-G5/S1.
Il vous suffit de régler la pression du ballonnet souhaitée, puis l'IntelliCuff prendra le relais pour surveiller et maintenir en continu la pression définie. La pression mesurée dans le ballonnet est affichée sous forme de valeur de monitorage.
En cas de détérioration du ballonnet, l'IntelliCuff déclenche une alarme tout en compensant les fuites pour sécuriser les voies aériennes.

Nous utilisons le dispositif IntelliCuff comme fonction standard de prévention de la BPAVM chez les patients ventilés mécaniquement. Le dispositif IntelliCuff contrôle automatiquement et régulièrement la pression du ballonnet. C'est une aide précieuse pour nous, le personnel soignant, car nous n'avons pas besoin de contrôler manuellement la pression du ballonnet toutes les heures.
Chef du département des soins infirmiers en USI
Hôpital du canton des Grisons, Coire, Suisse
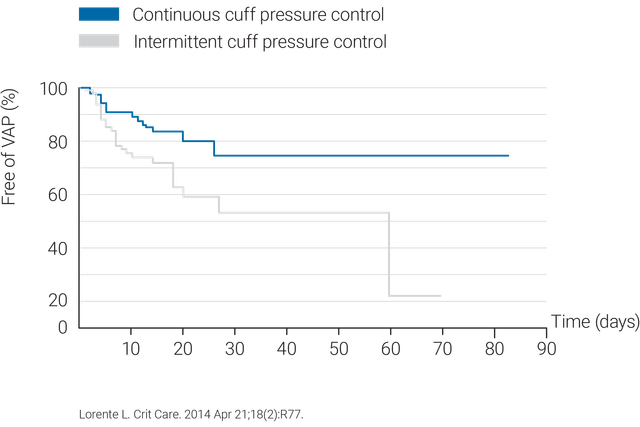
L'utilisation d'un système de contrôle continu de pression du ballonnet tel que l'IntelliCuff est plus efficace pour maintenir une pression du ballonnet dans une plage optimale (
Pour éviter des lésions de la trachée et des ulcères de pression, l'IntelliCuff est doté d'un réglage de pression du ballonnet par défaut défini sur 25 cmH2O (

L'IntelliCuff est disponible en tant que système autonome pour tous les ventilateurs ou en tant que solution intégrée en option sur le HAMILTON-C6 et le HAMILTON-G5, et de série sur le HAMILTON-S1.