Nosso modo de ventilação promove você de operador a supervisor. O INTELLiVENT-ASV reduz o número de interações manuais com o respirador (
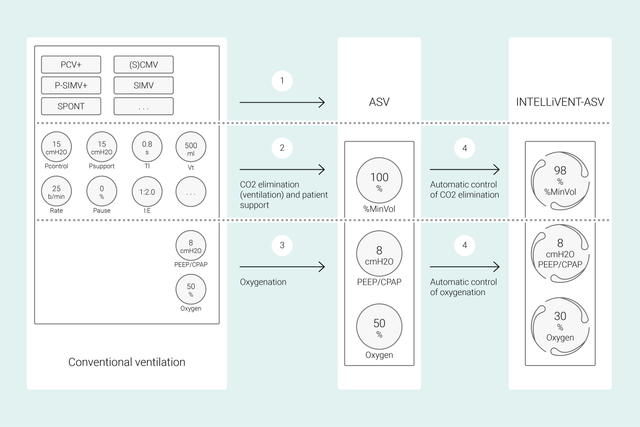
Em modos convencionais, você define os controles do respirador, tais como o volume corrente ou a pressão, a frequência respiratória, FiO2, PEEP, e o tempo inspiratório e expiratório, para alcançar determinados alvos clínicos. Adicionalmente, todos esses controles precisam ser reavaliados e ajustados com frequência.
Com o INTELLiVENT‑ASV, seus alvos clínicos definidos e estratégias para oxigenação e ventilação são o foco central. Depois de definir esses alvos, pode decidir em que medida o INTELLiVENT‑ASV deve controlar a oxigenação e a ventilação para alcançá-los.
O INTELLiVENT‑ASV seleciona automaticamente as configurações do respirador, gerencia a transição entre os estados passivo e ativo e apoia ativamente seus protocolos de desmame usando o Quick Wean.
Vários estudos internacionais demonstraram a segurança e o desempenho do INTELLiVENT-ASV em vários cenários clínicos — desde pós-cirurgia cardíaca (


Neste vídeo, o Dr. Jean-Michel Arnal, Senior Intensivist, apresenta uma rápida demonstração das principais funcionalidades e configurações da INTELLiVENT-ASV em um paciente real de UTI.
No início, defina a altura, o sexo e, se necessário, a condição específica do paciente: ARDS, Hipercapnia crônica, ou Lesão cerebral. Em seguida, defina os alvos clínicos em termos de oxigenação (SpO2) e eliminação de CO2 (PetCO2) para o seu paciente.
Dispõe de várias opções para ajustar o INTELLiVENT-ASV. Por exemplo, pode decidir se pretende definir a PEEP manualmente ou se pretende que a INTELLiVENT-ASV defina a PEEP dentro de um intervalo definido por você. Depois de revisar ou definir os limites de alarme, está pronto para iniciar a ventilação.
A INTELLiVENT-ASV implementa sua estratégia junto ao leito. Em vez de fazer alterações frequentes nas configurações individuais, monitore e reajuste as metas e a estratégia quando necessário.
A INTELLiVENT‑ASV visa manter o paciente dentro da intervalo-alvo definido e mantê-lo lá, ao mesmo tempo em que mantém a ventilação de proteção pulmonar (
Essas informações são medidas por três sensores: o sensor de fluxo proximal fornece dados sobre a mecânica pulmonar e a atividade do paciente, enquanto os sensores SpO2 e CO2 fornecem dados sobre oxigenação e eliminação de CO2.
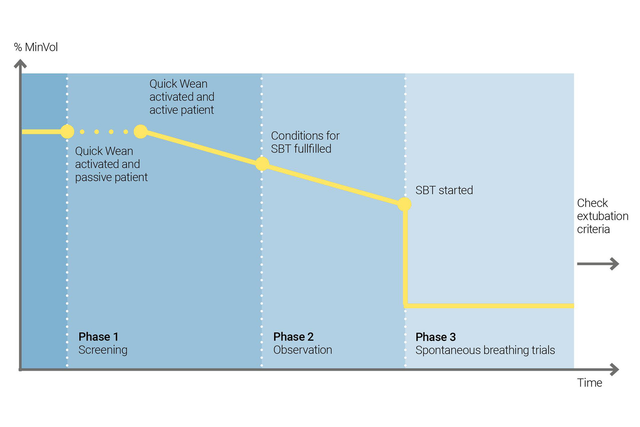
Use o Quick Wean da INTELLiVENT-ASV para implementar seu protocolo de desmame. Pode ativar o Quick Wean durante a ventilação quando o paciente estiver respirando espontaneamente.
Você pode configurar o Quick Wean ativando a SBT para avaliar a prontidão do seu paciente para ser separado do respirador. Ajuste os critérios para iniciar uma SBT, as configurações a serem usadas enquanto a SBT estiver em execução e os critérios para interrompê-la.
A INTELLiVENT‑ASV exibe sempre o histórico de todas as SBTs realizadas. Se uma SBT não for bem-sucedida, a INTELLiVENT‑ASV reverte para as configurações de ventilação anteriores.
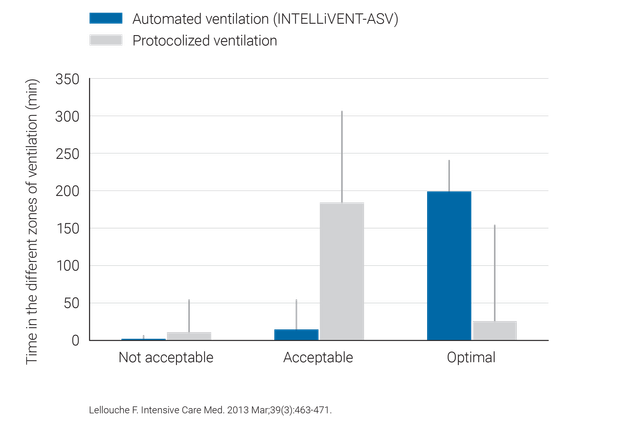
Estudos clínicos demonstraram que a INTELLiVENT-ASV seleciona uma pressão diferencial (
O INTELLiVENT-ASV requer menos ajustes manuais do que a ventilação convencional, reduzindo, consequentemente, a carga de trabalho da equipe de saúde (

A INTELLiVENT-ASV disponível como opção no HAMILTON-C6, HAMILTON-G5, HAMILTON-C3, HAMILTON-C1 e no HAMILTON-T1, e é um modo padrão no HAMILTON-S1.