
Autor: Bernhard Schmitt; Mirko Belliato, MD (Pavia, Italy)
Datum: 29.11.2022
Last change: 29.11.2022
English additions made in German version
Die turbinenbetriebenen Beatmungsgeräte können höhere kontinuierliche Flowraten verabreichen und die Luftzufuhr wird mit HEPA-gefilterter Raumluft mit Umgebungsfeuchtigkeit gespeist. Im Folgenden finden Sie eine schrittweise Anleitung zur Verwendung eines Helms für die NIPPV-Beatmungstherapie bei erwachsenen COVID-19-Patienten mit einem Beatmungsgerät von Hamilton Medical.
HINWEIS! Beatmungsgeräte von Hamilton Medical dürfen nicht für die CPAP-Therapie mit Helm verwendet werden.Stattdessen wird empfohlen, auf beiden Seiten des Helms ein ventilfreies System mit kontinuierlichem Flow zu verwenden (
ACHTUNG! Zwei beatmete Kompartimente in Folge = Helm + Lungen.
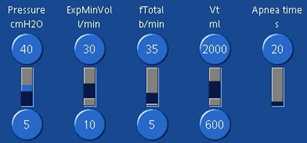
| Druckrampe | Auf die höchstmögliche Geschwindigkeit eingestellt |
| PEEP | PEEP-Zielwert + 30–50 % Minimaler PEEP-Wert = 10 mbar für einen steiferen Helm |
| Psupport | Psupport-Zielwert + 30–50 % Minimaler Psupport-Wert = 12 mbar |
| Trigger für die Inspiration | Mit 2 l/min beginnen und möglichst niedrig halten |
| ETS | Mit ETS-Standardeinstellung von 25 % beginnen, auf Asynchronien bei der Einleitung der Exspiration überwachen und entsprechend anpassen |
| Ti max | Auf 1,5 s einstellen, um eine späte Einleitung der Exspiration zu vermeiden |
| Sauerstoff | Mit einer Sauerstoffeinstellung von 60 % beginnen und auf Basis des SpO2-Werts titrieren Hinweis: Bei einer einzigen Gasquelle (100 % Sauerstoff) kann die Peakflow-Kapazität begrenzt sein. |
| Tidalvolumen | Zwischen 1.000 and 1.500 ml Hinweis: ~ 50–75 % des verabreichten Vt wird an den Helm verteilt! |
| ExspMinVol | > 25 l/min für eine ausreichende CO2-Auswaschung Die Wirksamkeit kann durch PCO2-Monitoring im Helm überwacht werden – siehe Tipps und Tricks unten. |
(Bildmaterial freundlicherweise zur Verfügung gestellt von Dr. Mirko Belliato, Policlinico San Matteo Pavia Fondazione IRCCS s.c. Anestesia e Rianimazione II Pavia, Italien.)
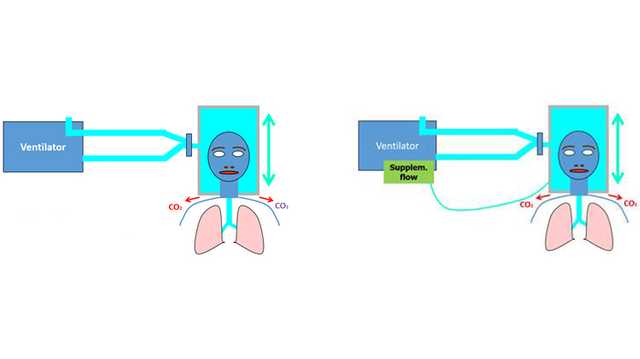
Wird Sauerstoff über einen Nasenkatheter, eine Maske oder nichtinvasive Beatmung (NIV) verabreicht, entweicht eine erhebliche Menge ausgeatmete Luft in die Umgebung. Das kann die Verteilung von Viren und damit das Risiko einer nosokomialen Infektion erhöhen (
Es besteht die Hoffnung, dass die Beatmung mit Helm zur Verminderung des Risikos für eine nosokomiale Infektion beitragen kann: In diesem Fall wird anstelle der Gesichtsmaske ein Helm für die Verabreichung der nichtinvasiven Beatmung verwendet. Ein Vergleich der NIPPV-Beatmung mit Helm mit der NIPPV-Beatmung mit Gesichtsmaske ergab in einer simulierten Umgebung mit einem Intensivbeatmungsgerät, einem Schlauchsystem mit zwei Schenkeln und einem Filter am Exspirationsanschluss des Beatmungsgerätes, dass die Leckage von ausgeatmeter Luft bei der Beatmung mit Helm vernachlässigbar war (
Dennoch mahnen einige Experten beim Einsatz von Helmen zur Vorsicht. In den Richtlinien der ESICM werden sie als ansprechende Option beschrieben, da sie nachweislich die Verteilung von ausgeatmeter Luft reduzieren. Die Autoren betonen aber, dass sie nicht sicher sind, was die Sicherheit und Wirksamkeit von Helmen bei COVID-19-Patienten angeht. Daher konnten sie keine Empfehlung zur Verwendung der NIPPV-Beatmung mit Helm gegenüber der NIPPV-Beatmung mit Maske aussprechen (
Aufgrund des weit höheren Volumens (immer höher als das Tidalvolumen) ähnelt ein Helm einer halbgeschlossenen Umgebung wie einem geschlossenen Raum mit einem Luftaustauschsystem. Geht man von einer homogenen Verteilung von CO2 aus, hängt die CO2-Konzentration in einer derartigen Umgebung vorrangig von zwei Faktoren ab: der CO2-Menge, die vom Probanden produziert wird (V˙CO2), und dem Flow von Frischgas, der der Umgebung zugeführt wird (
Hinweis!
Obwohl wir bei der Zusammenstellung der in diesem Handbuch enthaltenen Informationen größtmögliche Sorgfalt haben walten lassen, stellen diese keine offizielle Empfehlung durch das Unternehmen Hamilton Medical dar und können nicht an die Stelle der Meinung, Beurteilung und Anweisungen des ausgebildeten medizinischen Fachpersonals treten.
Vollständige Referenzen unten: (
Erhalten Sie einen Überblick über die Vorteile und klinische Relevanz der nichtinvasiven Beatmung sowie praktische Informationen zur Auswahl der richtigen Interface, Anpassung der Einstellungen und Überwachung des Patienten.