Le fasi, la forma e la morfologia della curva di un capnogramma volumetrico, insieme ai valori calcolati a partire dalle misure, possono dire molto su:
Sui nostri ventilatori, la CO2 viene misurata con un sensore mainstream di CO2 CAPNOSTAT-5 in posizione prossimale alle vie aeree del paziente.
Il sensore CAPNOSTAT-5 fornisce misure precise dell'end-tidal CO2 (PetCO2) e un capnogramma chiaro e accurato a tutte le frequenze respiratorie fino a 150 respiri al minuto.
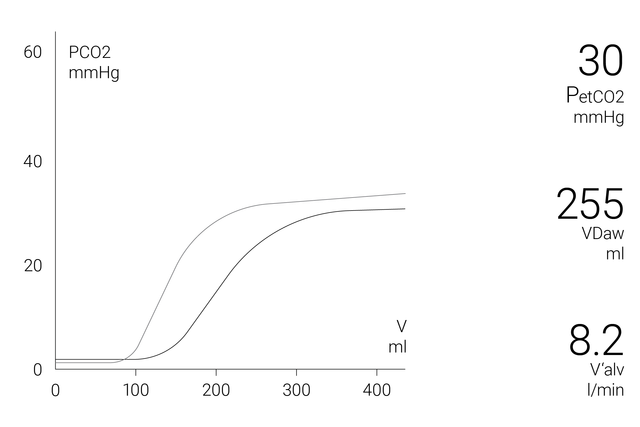
La finestra del capnogramma volumetrico sullo schermo mostra dati quantitativi esatti combinando i dati sul flusso prossimale e i dati sulla CO2, per esempio:
Per consentire un'analisi più completa delle condizioni del paziente, sono disponibili i trend su 72 ore (o su 96 ore con ventilatori HAMILTON-G5/S1) di:
Per semplificare le cose, i ventilatori Hamilton Medical offrono una panoramica di tutti i valori rilevanti legati alla CO2 nella finestra Monitoraggio CO2.
Tutto quel che serve per interpretare un capnogramma volumetrico e avere una panoramica dei vantaggi e delle applicazioni cliniche della capnografia volumetrica. Comprende un test da eseguire in autonomia!
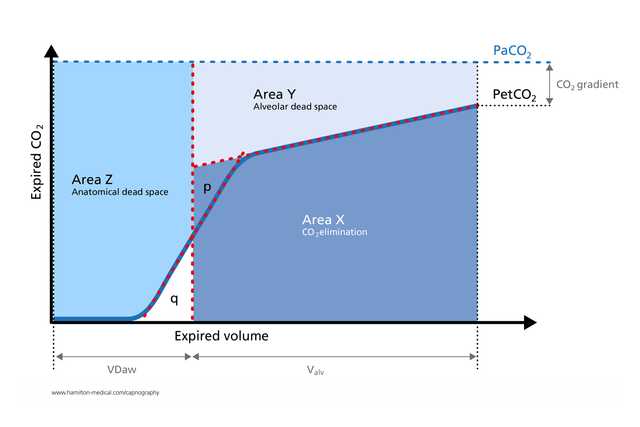
Il capnogramma volumetrico è stato utilizzato con risultati positivi per misurare lo spazio morto anatomico, la perfusione capillare polmonare e l'efficienza della ventilazione (
I valori calcolati sulla base della capnografia volumetrica sono utili per identificare un'eventuale embolia polmonare al posto letto (
In uno studio condotto su pazienti con ARDS sottoposti a ventilazione meccanica, le misure di capnografia volumetrica relative al rapporto tra spazio morto e volume corrente sono risultate accurate quanto i valori ottenuti con la tecnica del monitoraggio metabolico (
Il capnogramma espiratorio è un metodo di misurazione rapido, non invasivo e indipendente dallo sforzo respiratorio che agevola la rilevazione dei casi di broncospasmo significativo nei pazienti adulti con asma (
Poiché fornisce informazioni preziose e in tempo reale sulla fisiologia del collasso e del reclutamento polmonare in modo non invasivo, la capnografia volumetrica consente di monitorare le manovre di reclutamento cicliche al posto letto (

Mettiamo a disposizione prodotti di consumo originali per pazienti adulti, pediatrici e neonatali. È possibile scegliere tra prodotti riutilizzabili e monouso secondo le procedure stabilite dalla struttura sanitaria.
La capnografia volumetrica è disponibile come opzione sul ventilatore HAMILTON-C6, sul nuovo HAMILTON-C6 e sui modelli HAMILTON-C3 e HAMILTON-C1/T1.