
Le soluzioni convenzionali per la gestione della pressione di cuffia richiedono di monitorarla e regolarla manualmente.
Possono essere necessarie anche otto regolazioni al giorno per mantenere la pressione di cuffia sempre all'interno dell'intervallo desiderato (

IntelliCuff protegge le vie aeree del paziente (
È possibile utilizzarlo sia come dispositivo autonomo da associare a tutti i ventilatori meccanici, sia come soluzione integrata per i modelli HAMILTON-C6 e HAMILTON-G5/S1.
È sufficiente impostare la pressione di cuffia desiderata: IntelliCuff prende il controllo per monitorare costantemente e mantenere la pressione impostata. La pressione misurata nella cuffia è visualizzata come valore di monitoraggio.
Nell'eventualità che la cuffia sia danneggiata, IntelliCuff genera un allarme e continua a compensare la perdita per mantenere ferme le vie aeree.

Utilizziamo IntelliCuff come funzione standard per contribuire a evitare la VAP nei pazienti sottoposti a ventilazione meccanica. IntelliCuff controlla automaticamente e regolarmente la pressione di cuffia. È di grande aiuto al personale assistenziale, perché non dobbiamo controllare personalmente la pressione di cuffia ogni ora.
Responsabile infermeria di terapia intensiva
Ospedale cantonale dei Grigioni, Coira, Svizzera
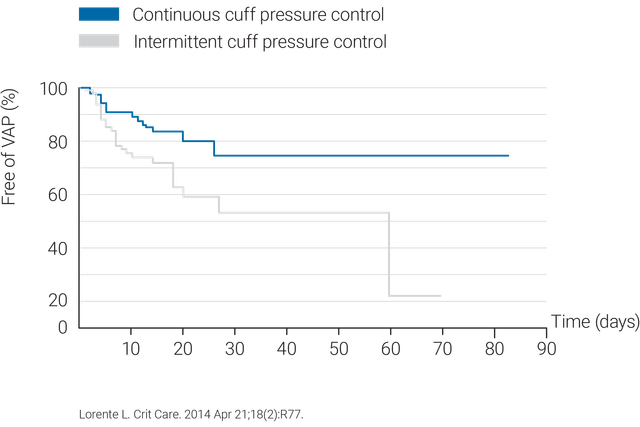
L'utilizzo di un sistema di controllo continuo della pressione di cuffia come IntelliCuff è più efficace nel mantenere la pressione di cuffia all'interno di un intervallo ottimale (
Per evitare lesioni tracheali e ulcere da pressione, IntelliCuff ha un'impostazione predefinita per la pressione di cuffia pari a 25 cmH2O (

IntelliCuff è disponibile come dispositivo autonomo per tutti i ventilatori o come soluzione integrata opzionale sui modelli HAMILTON-C6 e HAMILTON-G5; è inoltre di serie sul ventilatore HAMILTON-S1.