
我们的转运专家!从新生儿到成人






通信主板选项适用于:








各种方案适用于所有主要类型的直升机和救护车,以及医院病床、担架、台面、支架、杆、扶手和屋顶。
通过四种不同的手柄和多种安装架,HAMILTON-T1 便携型呼吸机可适应您的特定环境和情况。

如果您必须执行 CPR,则 CPR 通气自适应通气设置。其显示与情况相关的主要监测参数和曲线,并通过快速访问可预配置的设置、适当的报警和触发调节以及 CPR 计时器显示来支持您的工作流程。
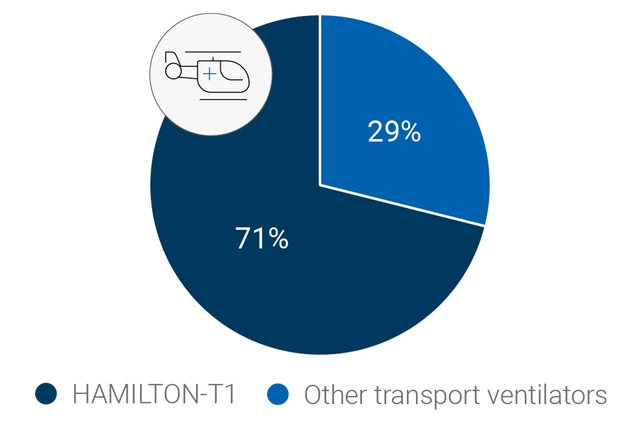
作为救护车、直升机等的转运呼吸机,HAMILTON-T1 是许多救援人员的最爱。根据 2019 年在德国、奥地利、瑞士、意大利和卢森堡的空中救援组织中开展的 HOVER 在线调查(

适合疫情大流行和大量伤亡的呼吸机必须是多功能的,而且满足各种要求。HAMILTON-T1 满足或超越 AARC 满足大流行流感和大量伤亡事故需求的呼吸机采购指南 (
从各个角度发现 HAMILTON-T1,点击热点,以了解更多信息。
| 病人组 | 成人/儿童、新生儿 |
|---|---|
| 外形尺寸(宽x深x高) | 320 x 220 x 270 mm(呼吸机主机) 630 x 630 x 1380 mm(无手柄) 630 x 630 x 1433 mm(带手柄) |
| 重量 | 6.5 kg(14.3 磅) 18.5 kg(40.8 磅)(含台车) |
| 监视器尺寸和分辨率 | 214 mm(8.4 英寸)对角线 640 x 480 像素 |
| 可拆卸式监视器 | |
| 电池运行时间 | 一块电池 4 小时 两块电池 8 小时 |
| 热插拔电池 | |
| 气源 | 集成涡轮 |
| O2 接头 | DISS 标准接口(CGA 1240 认证)或 NIST 通用接口 |
| 连接 | CO2/护士呼叫器/COM1、CO2/SpO2/COM1、CO2/SpO2/湿化器和 COM1、USB 端口、RJ-45 以太网端口 |
| 音量 | 43 dB(在正常运行情况下) |
| 容量控制、流量控制 | |
|---|---|
| 定量、适应性压力控制 | |
| Pressure-controlled | |
| 智能通气 | ASV®、INTELLiVENT®-ASV®(选项) |
| 无创通气 | |
| 高流量 | |
| 肺力学指标可视化(动态肺) | |
|---|---|
| 病人呼吸机依赖性可视化 | |
| 二氧化碳图 | |
| 氧饱和度监测 | |
| Lung stress and strain monitoring (Lung Impact panel) | |
| 食道压测量 |
| 肺复张性评估和肺复张 (P/V Tool Pro) | |
|---|---|
| 人机同步 (IntelliSync+) | |
| CPR 通气 | |
| Hamilton Connect 模块 | |
| Suctioning tool | |
| SpeakValve compatibility | |
| On-screen help | |
| O2 assist |
| 远程连接至 HAMILTON-H900 湿化器 | |
|---|---|
| 集成 IntelliCuff 气囊压力控制器 | |
| 集成气动雾化器 | |
| 集成 Aerogen 雾化器 | |
| 与 Sedaconda ACD-S 麻醉剂输送系统的兼容性 |

暴露于极端环境意味着军用呼吸机必须满足非常特殊的要求。这是 HAMILTON-T1 的用途所在。
根据病人的肺力学指标和呼吸用力,ASV 通气模式每天 24 时从插管到拔管连续调整每次呼吸时的呼吸频率、潮气量和吸气时间。
INTELLiVENT-ASV 智能通气模式持续调整病人的通气和氧合状态。
它根据临床医生设定的目标值和病人的生理输入设置分钟通气量、PEEP 和氧浓度。
O2 assist 是一项先进的氧疗管理技术,可在床旁为您提供精准护理。通过持续调节供氧水平,将病人的氧饱和度 (SpO2) 水平始终维持在个体化设定的目标范围内。该功能可减少操作旋钮的次数(
无创通气模式提供压力支持流速切换的自主呼吸(NIV 和 NIV-ST 模式)和压力控制时间切换的指令呼吸 (NIV-ST)。
与使用压缩空气的呼吸机相比,我们的涡轮驱动呼吸机能够提供更高的峰值流量。这就保证了即便漏气严重也具有最佳性能。
高流量鼻导管治疗(
我们的独立高流量氧疗设备 HAMILTON-HF90 同样提供了此疗法 (
在 nCPAP 模式下,病人通过持续气道正压通气获得支持。在我们的流量控制型设备中,目标 CPAP 值通过调节呼吸气体流量进行设定。为补偿可能发生的漏气(例如经口或鼻腔漏气),可启用 LeakAssist 功能。该能够可通过补充呼吸气体流量维持预设的气道压力。
集成气动雾化器完全与吸气和呼气时间同步。
集成同步 Aerogen 雾化系统作为一个选配件提供 (
输送药物气溶胶粒子的细水雾有助于您恢复支气管痉挛、提高通气效率和减少高碳酸血症 (
IntelliSync+ 通过每秒数百次波形持续分析波形,能够立即检测病人用力和循环,并实时启动吸气和呼气。
IntelliSync+ 适用于有创和无创通气,无论采用哪种通气模式。
通过独特的呼吸机连接选项可以直接从呼吸机的显示屏上操作 HAMILTON-H900 湿化器(
湿化器也可以根据所选的通气模式自动选择湿化模式(有创、无创或高流量)。
说话瓣膜选项让气管切开的病人说话,而且允许他们甚至在接受通气治疗时吞咽。
调节呼吸机的监测、触发和报警管理,以在压力控制模式 (PCV+, SPONT, PSIMV+) 下与说话瓣膜兼容。
近端流速和二氧化碳测量使我们的呼吸机能生成最新的容积二氧化碳图,为评估通气质量和新陈代谢活动提供生要依据。
通气状态面板显示与病人的呼吸机依赖性相关的六个参数,包括氧合状态、CO2 清除状态和病人活动。
各栏中上下移动的浮动指示器显示给定参数的当前值。
快速撤机是 INTELLiVENT-ASV 模式的一个功能,其可提供对病人状况的持续动态监测和控制,从而评估病人是否适于拔管。
动态肺面板向您显示下列重要监测数据的实时图表视图:
呼吸机可根据所选的监测参数组合显示动态环图。有了趋势图功能,您可以看到针对您选择的监测参数和时间框所显示的趋势数据。
设备持续将监测参数保存在其存储器中,即使在待机时也不停止。
氧饱和度选项提供集成无创氧饱和度测量,数据方便地显示在您的呼吸机上。
我们还提供氧饱和度传感器的全面组合方案。

我们预组装的呼吸装置包括操作呼吸机所需的基本耗材,而且方便地放在一个包装袋中。
我们的所有基本耗材都专门为保证制造商质量的 Hamilton Medical 哈美顿医疗公司呼吸机开发。

为管理通气,您通常需要设置多个参数,例如,压力、容量、吸气和呼气触发、气囊压力等。每次您的病人状况改变时,您需要进行一次或多次调节。
为简化此过程和减少人工操作,我们创建了一系列解决方案:
适应性支持通气 (ASV) 是一种根据病人的肺力学指标和呼吸用力连续适应呼吸频率、潮气量和吸气时间的通气模式。研究表明,ASV 可缩短各种人群的机械通气时间,而且手动设置更少 (
我们的智能通气模式 INTELLiVENT-ASV 使您从操作者转变为监督者,减少与呼吸机手动互动的次数 (
气囊压力管理的常规解决方案需要您手动监测和调节气囊压力。
IntelliCuff 通过连续测量和自动维持所设置的成人、儿童和新生儿病人的气囊压力,安全管理病人的气道 (
O2 assist is an advanced oxygen management technology that acts as your precision-care assistant at the bedside. By continuously adjusting the oxygen supply, it maintains the patient’s SpO2 levels within the individually set target ranges. This ensures less knob-turning for you (

无论何时出现问题,呼吸机都会利用报警灯、声音和信息栏警示您。
屏幕上的帮助内容向您提供有关如何解决报警的建议。

我们的在线学院提供易于遵循的学习路径,以使您尽快熟悉 Hamilton Medical 哈美顿医疗公司产品和技术。
我们不断努力进一步革新我们的产品。添加新的功能和改善现有功能,以确保您在您的呼吸机寿命期间始终拥有最新的通气技术。


无论用于 ICU、MRI 科室或病人转运,所有 Hamilton Medical 哈美顿医疗公司呼吸机的用户界面操作方式均相同。
我们的通气酷屏将复杂的数据集成到直观的可视化图像。
我们围绕最高病人安全性和易用性开发我们的附件。我们尽可能将附件集成到我们的呼吸机,以简化整个呼吸机系统的操作。

我们的通气极客团队很乐意帮助您选择最适合您临床护理环境的通气设备,并帮助您实现治疗目标。获取个性化报价或安排电话回访,了解更多信息。